Splenic marginal zone lymphoma
This information is about splenic marginal zone lymphoma – a slow-growing type of non-Hodgkin lymphoma that develops in the spleen.
On this page
What is splenic marginal zone lymphoma?
What is splenic marginal zone lymphoma?
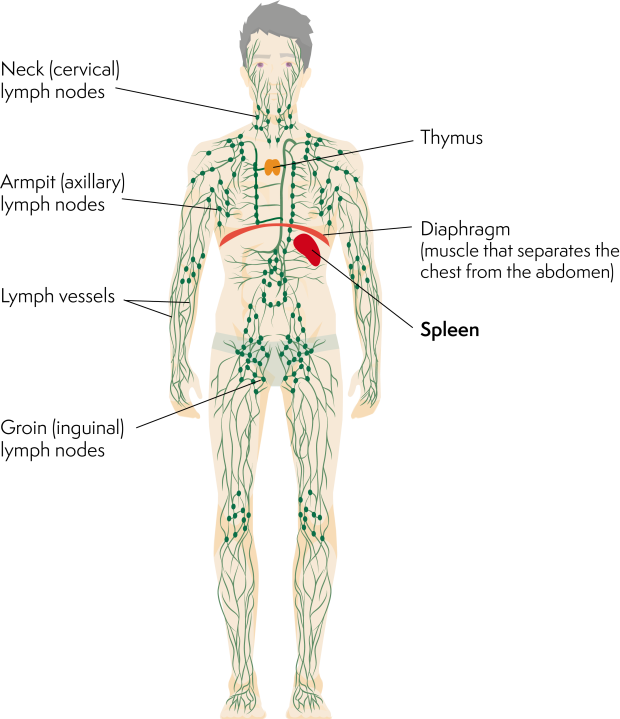
Lymphoma is a type of blood cancer that develops when white blood cells called lymphocytes grow out of control. Lymphocytes are part of your immune system. They travel around your body in your lymphatic system, helping fight infections. There are two types of lymphocyte: B lymphocytes (B cells) and T lymphocytes (T cells).
Lymphomas can be grouped as Hodgkin lymphomas or non-Hodgkin lymphomas, depending on the types of cell they contain. Marginal zone lymphomas are types of slow-growing (low-grade) non-Hodgkin lymphomas that develop from B cells. They are called marginal zone lymphomas because they develop in a particular region at the edge of lymphoid tissues (collections of lymphocytes) called the marginal zone.
There are three types of marginal zone lymphoma:
- splenic marginal zone lymphoma, which develops in the spleen
- nodal marginal zone lymphoma, which develops in lymph nodes
- MALT lymphoma (extranodal marginal zone lymphoma), which develops in lymphoid tissue outside lymph nodes.
Splenic marginal zone lymphoma (often called splenic MZL) develops when abnormal B cells collect in your spleen.
What is the spleen?
The spleen is part of your immune system. It’s normally about the size of a pear and it lies just under your rib cage on the left-hand side of your body. It is involved in fighting infections, filtering your blood and removing old blood cells. You can’t normally feel your spleen, but a swollen (enlarged) spleen might feel like a lump at the top left of your tummy.
Who gets splenic marginal zone lymphoma?
Splenic MZL is rare. It accounts for fewer than 2 in every 100 cases of non-Hodgkin lymphoma. Splenic MZL can affect people of any age but it is most common in people in their 60s.
In most cases, it is not known what causes splenic MZL. It is more common in people who have been infected with hepatitis C virus and some autoimmune conditions. However, the vast majority of people who have had hepatitis C or autoimmune conditions do not go on to develop lymphoma.
Symptoms of splenic marginal zone lymphoma
Splenic MZL might not cause any symptoms at all but your doctor might notice that your spleen is bigger than it should be during a routine examination, or find abnormal cells when you have a blood test done for another reason.
In most people, splenic MZL causes enlargement of your spleen. This is called ‘splenomegaly’. If your spleen becomes very big, you might feel full very quickly when you eat, or get pain or discomfort behind your ribs.
It is important to note that most people with an enlarged spleen do not have lymphoma. The NHS has more information on problems affecting the spleen.
Unlike most lymphomas, splenic MZL does not usually cause swollen lymph nodes.
Some people experience unexplained weight loss, night sweats or fever. These are known as ‘B symptoms’ and often occur together.
Some people with splenic MZL have symptoms caused by lymphoma in their bone marrow (the spongy tissue in the centre of bones where blood cells are made). These include:
- anaemia (a shortage of red blood cells), which can make you feel tired or short of breath
- thrombocytopenia (a shortage of platelets), which can cause you to bruise or bleed more easily than usual.
Around 1 in 5 people with splenic MZL produce abnormal antibodies that clump together at lower temperatures. These are called ‘cryoglobulins’. This can lead to many symptoms, including poor circulation or a rash, especially when it is cold.
Diagnosis and staging of splenic marginal zone lymphoma
Splenic MZL can be difficult to diagnose. It can look similar to other types of lymphoma, such as Waldenström’s macroglobulinaemia. It is usually diagnosed using a combination of:
- blood tests to check your blood cell counts and look for abnormal lymphocytes and antibodies in your blood
- a bone marrow biopsy (a test that involves taking a sample of bone marrow, usually from your hip bone) to check for lymphoma cells in your bone marrow.
The blood sample and bone marrow biopsy are examined by an expert pathologist. The pathologist also tests the samples for particular proteins that are found on the surface of lymphoma cells. This can help your medical team decide on the most appropriate treatment for you based on your lymphoma diagnosis.
If you have an enlarged spleen, your medical team might suggest that you have it removed so it can be tested in a laboratory to help make a diagnosis. This is done by an operation called a ‘splenectomy’. You can live without a spleen but you are less able to fight infections, so you need to take precautions to lower your risk of getting infections.
You also have blood tests to look at your general health, make sure your kidneys and liver are working well and test for infections such as hepatitis C virus.
You have other tests to find out which areas of your body are affected by lymphoma. This is called staging. It usually involves having a CT scan. You might also have a PET scan if your specialist thinks it would be helpful in planning your treatment, although this is less common for marginal zone lymphomas than other types of lymphoma.
You usually have your tests done as an outpatient. It takes a few weeks to get all the results. Waiting for test results can be a worrying time, but it is important for your medical team to gather all of this information in order to plan the best treatment for you.
Most people with splenic MZL have lymphoma in their bone marrow when it is diagnosed. This means it is usually advanced (stage 4). Effective treatment is available for advanced splenic MZL.
I was relieved that they had found something and that now they could do something to help me
Read more about Emma's story.
Outlook for splenic marginal zone lymphoma
Splenic MZL develops slowly. Treatment is often successful, but the lymphoma often relapses (comes back) and needs more treatment to keep it under control. Most people live with this type of lymphoma for many years. You might have periods when you feel well and don’t need treatment, and other periods when your symptoms get worse and you need more treatment.
Your medical team is best placed to advise you on your outlook based on your individual circumstances.
Transformation
Occasionally, splenic MZL can change (transform) into a faster-growing type of lymphoma. This happens in less than 2 in every 10 people with splenic MZL.
If your medical team thinks your lymphoma might have transformed, you might have a biopsy to check for faster-growing cells. Transformed splenic MZL lymphoma is treated in the same way as fast-growing (high-grade) non-Hodgkin lymphoma, such as diffuse large B-cell lymphoma (DLBCL).
Treatment for splenic marginal zone lymphoma
The treatment you have for splenic MZL depends on how the lymphoma is affecting you, your blood counts and your general health.
If you have hepatitis C virus, you are likely to be offered anti-viral treatment. Clearing the infection might also clear the lymphoma. If this is the case, you might not need any more treatment.
Active monitoring
If your lymphoma is not causing troublesome symptoms and your blood counts are not too low, you might not need treatment straight away. Instead, your medical team might suggest monitoring your symptoms and blood counts closely and saving treatment until it is needed. This is called active monitoring or ‘watch and wait’. This approach allows you to avoid the side effects of treatment for as long as possible. Delaying treatment in this way does not affect how well it works when you do need it, or how long you might live.
Around 1 in 3 people with splenic MZL do not have any symptoms when they are diagnosed and often do not need treatment for many years.
Treatment options
If you have troublesome symptoms or low blood counts, your medical team is likely to suggest that you start treatment. Splenic MZL is rare. This makes it difficult to determine exactly which treatment gives the best outcome.
The most common treatment for splenic MZL is antibody therapy such as rituximab. This is often given on its own for splenic MZL. It can be very effective. You might have an initial course of rituximab to put your lymphoma into remission, followed by maintenance therapy to make your remission last as long as possible.
Some people with splenic MZL have rituximab combined with chemotherapy. This is called ‘chemo-immunotherapy’. Combinations that might be used include:
- rituximab plus bendamustine
- rituximab plus chlorambucil
- rituximab plus CVP (R-CVP)
- rituximab plus CHOP (R-CHOP).
However, your medical team might recommend a different regimen (combination of drugs), or they might ask you if you’d like to take part in a clinical trial.
If your spleen is very enlarged and your blood counts are very low, your medical team might recommend that you have an operation to remove your spleen (a splenectomy), if you haven’t had it removed already. This can relieve symptoms very quickly. After having your spleen removed, your body is less able to fight infections, so you need to take precautions to reduce your risk of getting infections. You are likely to have long-term antibiotic treatment.
If you have symptoms caused by abnormal antibodies in your bloodstream, you are likely to be treated with steroids. These might be part of your chemotherapy regimen.
Side effects of treatment
Treatments affect people differently. Each type of treatment or drug has a different set of possible side effects. Your medical team should give you information about the side effects associated with any treatment they recommend for you. Ask for more information if you are worried about potential side effects. Your medical team can offer advice or prescribe medicines if you experience troublesome side effects during your lymphoma treatment.
Follow-up of splenic marginal zone lymphoma
When you are in remission (disappearance or significant shrinkage of lymphoma) after your treatment, or during a period of active monitoring (watch and wait), you have regular follow-up appointments in the clinic.
Your follow-up appointments are to check that:
- you are recovering well from treatment
- you have no signs of the lymphoma coming back (relapsing) or getting worse
- you are not developing any late effects (side effects that develop months or years after treatment).
At each appointment, your medical team will ask about any concerns or symptoms you have. You might have blood tests and a physical examination. You are unlikely to have a scan unless you have troubling symptoms.
Jackie talks about her experience of active monitoring after having a splenectomy for splenic MZL.
Relapsed or refractory splenic marginal zone lymphoma
It is common for splenic MZL to come back (relapse) after successful treatment. You can usually have more treatment to give another period of remission. This approach can often control the lymphoma for many years.
The treatment you have for relapsed or refractory splenic MZL depends on what treatment you’ve already had, and how long you responded to it:
- You might have rituximab with or without chemotherapy
- If you’ve had rituximab before and you didn’t respond to it, or if your response to treatment didn’t last long, you might be offered a splenectomy, if you haven’t already had one.
- Alternatively, you might be offered the targeted treatment zanubrutinib. Targeted treatments are medicines that have been specially designed to attack proteins that are important in helping the lymphoma cells to grow ad survive. Zanubrutinib is a type of targeted treatment called a BTK-inhibitor because it blocks a protein called Bruton’s tyrosine kinase.
Very occasionally, your medical team might recommend that you have a stem cell transplant using your own stem cells (an ‘autologous’ stem cell transplant). Stem cell transplants are usually only considered for splenic MZL if you have lymphoma that relapses very soon after treatment. Stem cell transplants are a very intense form of treatment and you have to be well enough to have one. A stem cell transplant allows you to have very high doses of chemotherapy. It might give you a better chance of having a long-lasting remission than standard chemotherapy regimens.
Research and targeted treatments
Splenic MZL is rare so most clinical trials include people with splenic MZL alongside other types of low-grade lymphoma.
There are several types of treatment being tested in clinical trials for marginal zone lymphomas, including drugs already approved for other types of lymphoma. These include:
- B-cell receptor pathway inhibitors, including other BTK inhibitors, which block signals involved in the growth and survival of lymphoma cells
- proteasome inhibitors which disrupt the balance of proteins in lymphoma cells
- BCL-2 inhibitors which activate the process of natural cell death
- immunomodulators which change how your immune system responds to lymphoma cells
- antibody treatments which bind to proteins on the surface of lymphoma cells to help your own immune system destroy them
- CAR T-cell therapy which uses modified cells from your own immune system to fight lymphoma.
Some of these might be available to you through a clinical trial. If you are interested in taking part in a clinical trial, ask your doctor if there is a trial that might be suitable for you. To find out more about clinical trials or to search for a trial that might be suitable for you, visit Lymphoma TrialsLink.
