CT and PET/CT scan
CT and PET/CT scans are often used in helping to diagnose and treat lymphoma.
We have separate information about being referred for tests and scans, ultrasound and X-ray scans, MRI scan, and waiting for test results. You might also be interested in our video about scans for lymphoma.
On this page
Frequently asked questions about CT and PET/CT scans and lymphoma
What is a CT scan?
A computed tomography (CT or CAT) scan uses lots of X-rays to take pictures through your body. CT scans can be helpful in taking pictures of internal organs, including lymph nodes.
They take images as ‘slices’ through your body in any direction. The X-ray images show on a computer screen.
CT scans can help to:
- diagnose lymphoma
- work out how many and which areas of your body are affected by lymphoma (known as your lymphoma stage)
- find the best place to take a biopsy
- plan radiotherapy treatment
- check response to treatment, by comparing scans taken before, during and at the end of a course of treatment
- find out if your lymphoma has come back (relapsed) if you have symptoms that could suggest it has.
You can find out more about CT scans on the Radiology info.org website.
PET/CT scans
PET stands for positron emission tomography. A PET/CT scan is where you have both a CT scan and a PET scan in the same appointment. This can help to give a clearer picture of which areas of your body are affected by lymphoma. In some cases, you might have a PET scan alone. Your doctor will choose the most suitable scan for you.
PET scans
PET scans use a harmless radioactive form of sugar (radiotracer) to look at how active the cells in your body are. Lymphoma cells are quite active, so take up quite a lot of sugar. A special camera recognises the radioactivity in the cells, which shows up as ‘hot spots’ on the scan image.
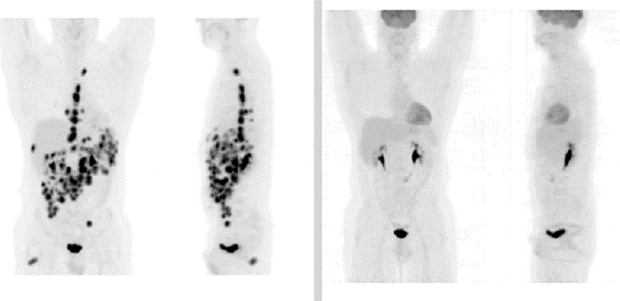
© The Royal Marsden NHS Foundation Trust
Fluoro-deoxy-glucose (FDG) is the radiotracer most often used in PET scans. Sometimes, it’s called an FDG-PET. You have FDG as an injection into a vein before your PET scan. Side effects from the injection are uncommon and generally very mild. Your hospital team should talk to you about these beforehand.
PET scans can be useful:
- before treatment, to help work out which parts of your body are affected by the lymphoma (known as the stage of the lymphoma)
- after a few cycles of treatment, to help plan the next part of treatment
- at the end of your treatment, to check your lymphoma responded to it
- to find out if your lymphoma has come back (relapsed) if you have symptoms that could suggest it has.
If you need a PET scan after treatment, doctors usually recommend waiting:
- 3 to 4 weeks after finishing a course of chemotherapy
- around 3 months after finishing a course of radiotherapy.
This is because there might still be some activity where the lymphoma was, which could confuse the results.
Preparing for a scan
You’ll be given information in advance about how to prepare for your scan, including about:
- Medication – your medical team should tell you if it’s safe to have any of your usual medication before your scan. If you are having a PET scan and you are taking medication for diabetes, check with your hospital team. They might advise you not to take tablets or insulin for a number of hours before the scan.
- Food – your medical team will tell you if you can eat normally before your scan, or whether you need to stop eating (known as fasting) for a while beforehand. If you have diabetes, you’ll be given advice about eating.
- Drink – your medical team will tell you any specific instructions about if, when and how much to drink before your scan.
- Physical activity – you might be asked not to do strenuous exercise in the 24 hours before a PET/CT scan. This is because it can increase the uptake of the radiotracer and therefore affect the results.
The instructions specific to you and the type of scan you are having will be on your appointment letter so please read it carefully. If you have any questions about your scan before the day, contact the hospital.
Having a scan
Usually, you have a scan in the radiology or nuclear medicine department of a hospital, as an outpatient. If your local hospital doesn’t have a PET/CT scanning machine, you might need to travel to a hospital further away. Sometimes, however, it’s possible to have one at a mobile unit.

- On the day of your scan, the staff in the scanning department ask you whether you are, or could be pregnant.
- You might be asked to take off any metal you’re wearing, for example items with a zip, jewellery, belt, watch, or an underwired bra. If you wear glasses or coloured contact lenses, you might need to remove these too.
- If you are having a contrast agent , the hospital might ask that you arrive at your appointment an hour before your scan. This is to allow time for them to ask you questions about your general health, to check that it’s safe for you to have the contrast agent.
A PET/CT scan usually takes 30 to 60 minutes. However, you’re likely to be in the scanning department for 2 to 3 hours. You have your radiotracer injection and then wait for 60 to 90 minutes before having the scan. This allows time for your cells to take up the radiotracer.
To have your scan, you lie on a couch that moves slowly into the scanner. The scanning machine never surrounds your whole body at any one time.
- Once you are in the scanner, the hospital staff leave the room. They can see you from behind a screen and a video camera. You can speak to one another through a two-way speaker. You can raise your hand if you need to ask for help at any time.
- You need to keep very still during the scan. You might be asked to hold your breath for a few seconds at a time to help you stay still.
You can usually go straight home after the scan. However:
- You might be asked to stay in the hospital for a short time after a CT scan if you have had contrast agent through an injection. This allows time for hospital staff to check for any signs of an allergic reaction.
- You should avoid close contact with pregnant women, babies and young children for 6 hours after your PET/CT scan. This is because you still have some radioactivity in your body from the radiotracer. Most of it will leave your body after about 6 hours.
Airports and seaports
Airports and sea ports often have radiation alarms that could be set off by even very small levels of radiotracer left in your system.
If you travel by air or sea within a few days of having your scan, it could be helpful to take something with you to explain this. You could take your appointment letter or other official confirmation from the department where you had your scan.
Contrast agents
A contrast agent is a type of dye. It helps to show structures inside your body (blood vessels, organs and tissues) clearly. This can help to improve the quality of the scan image.
The type of contrast agent you have depends on which part of your body needs to be scanned.
Depending on the type of contrast agent, you might experience the following:
- warmth travelling down your arms
- a strange taste in your mouth
- feeling as though you need to wee
- feeling sick or dizzy.
These usually pass within a few minutes.
You usually have a contrast agent by injection. It can sometimes sting where the needle goes in. You might feel warm or cold where the contrast is injected.
Are there any side effects of having a contrast agent?
Side effects from contrast agents are uncommon. The risk of having an allergic reaction is small.
Allergic reactions
There is a small risk of having an allergic reaction to a contrast agent. Staff monitor you carefully and are trained to treat any allergic reactions quickly.
In general, allergic reactions to contrast agents are mild and include symptoms such as hives, a rash or swelling. However, in more severe cases, they could cause itchy skin, swollen lumps and breathing difficulties.
Before you have the contrast agent, hospital staff check your medical notes and ask you whether you have:
- certain conditions (for example kidney problems)
- particular allergies
- had an allergic reaction to a contrast agent in the past.
These factors could increase your risk of developing an allergic reaction to the contrast agent so you might have your scan without one.
Frequently asked questions about CT and PET/CT scans for lymphoma
Below are some questions people often ask about scans and lymphoma. Speak to your medical team for advice specific to your situation.
Who carries out the scan?
A radiographer carries out the scan.
Can I take someone with me to my scan?
You can take someone, such as a friend or family member, to the hospital with you. However, for most scans, they will need to wait in a different room while you have your scan.
Are CT and PET/CT scans safe?
CT and PET/CT scans use a type of energy called radiation.
Although high levels of radiation can cause cancer, the risk of developing cancer from the level of radiation used in medical scans is extremely low. Doctors weigh up the possible risks and benefits before they decide to do any type of scan.
Will I be radioactive after a scan?
With a PET or a PET/CT scan, you will give off very low levels of radiation for around 6 hours afterwards. As a precaution, you should avoid being close to women who are pregnant during this time. It should be safe to be around adult pets, as long as they are not pregnant.
Can I have a scan if I am pregnant?
There is a small risk to the development of an unborn baby from a CT or PET/CT scan, especially during the first trimester of pregnancy.
If you are pregnant, you might have a different type of scan, for example an ultrasound scan or a magnetic resonance imaging (MRI) scan.
Is it safe to breastfeed after my scan?
Talk to your doctors for advice. If you have only a CT scan, in general, it’s considered safe to breastfeed afterwards, including if you’ve had a contrast agent.
If you have a PET/CT scan, you might be advised to stop for a short while after having the radiotracer injection. If it is possible, you could consider expressing milk beforehand so that somebody else can feed your baby for a few hours after you have the scan.
Are scans painful?
Scans aren’t painful. However, some people find them uncomfortable if they need to stay still for a long time.
If you think you’ll find it difficult to lie still for long enough, talk to your doctor or another member of hospital staff before the day of your scan. They might suggest using support pillows to help keep you as comfortable as possible. In some cases, they might suggest that you take pain relief medication beforehand if lying still is likely to cause you discomfort. You could also talk to the radiographer on the day to help you find the most comfortable position for you.
What should I do if I feel anxious about having a scan?
Talk to a member of your medical team if you feel anxious about having a scan. They can answer any questions you have and might suggest ways of coping with your anxiety.
If you feel very anxious, you might be able to have an anti-anxiety drug before your scan. If you think this could help you, talk to the staff in the scanning department before the day of your appointment about this possibility. If you have an anti-anxiety drug, you should not drive for the rest of the day, so you might need to arrange transport home from your scan.
Can I have a scan if I have diabetes?
If you have diabetes, you might be given specific advice about what to eat on the day of your scan. You'll also be given information about how to take your medication. In some cases, your scan might be planned around your usual blood sugar levels.
When will I get the results of the scan?
Your medical team should be able to give you an idea of when to expect your test results. Staff in the scanning department won’t be able to give you your scan results while you’re at the hospital.
The person doing the scan isn’t usually trained to understand what the images mean. Instead, this information needs to be sent to a specialist.
The expert uses the scan and the results of all your other tests to help them work out what your scan pictures mean.
For some people, waiting for test results can be a particularly anxious time. Although the wait might feel long, it is important that doctors collect all of the information they need so that they can plan the best treatment for you. If you’d like to talk about how you’re feeling, our helpline team is here to support you.
Will I have scans during follow-up?
You might have a scan at the end of your treatment to check how well your lymphoma has responded. They are not routinely used as part of follow-up as there is no evidence to suggest that follow-up scans for lymphoma change lymphoma treatment or outcomes.
