Stem cell transplants
This page gives an overview of stem cell transplants in the treatment of lymphoma and outlines the difference between a self (autologous) stem cell transplant and a donor (allogeneic) stem cell transplant.
On this page
What is a stem cell transplant?
Why are stem cell transplants used?
When are stem cell transplants used?
Self (autologous) and donor (allogeneic) stem cell transplant?
What are stem cells?
Every day, your body makes more than 300 billion new blood cells to replace cells that die off naturally. There are three main types of blood cell:
- white blood cells (leucocytes) including lymphocytes, the cells that are abnormal in lymphoma and fight infection
- red blood cells (erythrocytes), which carry oxygen around your body
- platelets (thrombocytes), which help your blood to clot if you have an injury.
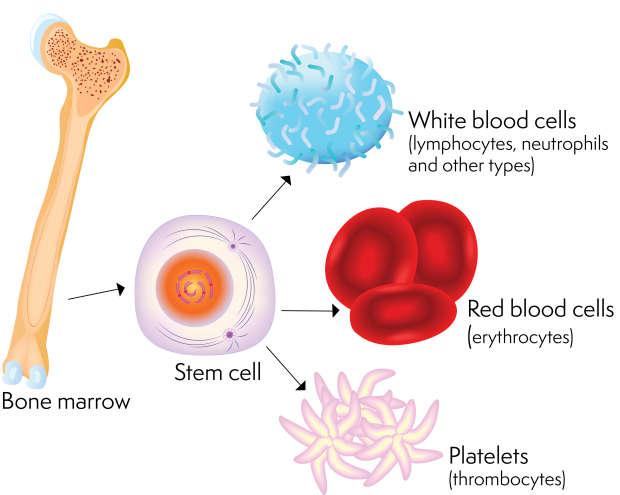
All these different types of blood cell develop in your bone marrow from blood (haemopoietic) stem cells. Stem cells are undeveloped cells that can divide and mature into all the different types of blood cell your body needs.
What is a stem cell transplant?
A stem cell transplant is a procedure that replaces damaged or destroyed stem cells in your bone marrow with healthy stem cells.
It is sometimes called a ‘peripheral blood stem cell transplant’ (if the healthy stem cells are collected from the bloodstream) or a ‘bone marrow transplant’ (if the healthy stem cells are collected from the bone marrow). Most stem cell transplants nowadays use stem cells collected from the bloodstream. We refer to both as ‘stem cell transplants’ in the rest of our information.
For detailed information on what stem cell transplants involve, see our separate pages on having a stem cell transplant, and self (autologous) stem cell transplants and donor (allogeneic) stem cell transplants.
Why are stem cell transplants used to treat lymphoma?
Stem cells are dividing all the time to create the blood cells your body needs. They are very sensitive to the effects of chemotherapy, which kills cells that are actively dividing.
When chemotherapy damages or destroys the stem cells in your bone marrow, your body cannot produce all the blood cells it needs. This might lead to:
- a low white blood cell count, especially a type of white blood cell called a neutrophil (neutropenia)
- a low red blood cell count (anaemia)
- a low platelet count (thrombocytopenia).
These low blood counts can cause serious side effects that sometimes mean you have to have a lower dose or shorter course of chemotherapy than planned.
Cycles of chemotherapy usually include rest periods so your bone marrow and blood counts can recover between treatments. However, some people need high doses of chemotherapy to treat their lymphoma. High doses of chemotherapy can be very effective at killing lymphoma cells but they can cause permanent damage to your stem cells.
A stem cell transplant allows you to be treated with a higher dose of chemotherapy than you would usually be able to have because it replaces the stem cells damaged by the chemotherapy. This allows your bone marrow to recover and make all the new blood cells that your body needs. If you have a stem cell transplant using cells from a donor (an ‘allogeneic’ stem cell transplant), it can also build a ‘new’ immune system that can help your body recognise and fight the lymphoma.
Stem cell transplants involve high-dose chemotherapy. Even after a stem cell transplant, it can take your bone marrow around 2 to 3 weeks to recover, although it can be more or less than this. It can take much longer – several months or more – for you to fully recover.
When might stem cell transplants be used to treat lymphoma?
Stem cell transplants are an intensive form of treatment and you have to be well enough to have one. They can be used to treat some types of Hodgkin lymphoma, high-grade non-Hodgkin lymphoma and low-grade non-Hodgkin lymphoma. Whether or not you need a stem cell transplant depends on lots of different factors, including the type of lymphoma you have, how your lymphoma responds to treatment and how well you are.
In general, stem cell transplants might be used if:
- your medical team thinks your lymphoma is very likely to come back (relapse) after treatment
- your lymphoma doesn’t respond to treatment (refractory lymphoma)
- your lymphoma has relapsed after treatment.
In these circumstances, a stem cell transplant might increase your chance of having a longer-lasting remission from lymphoma.
By the time of the transplant I was feeling better and stronger. I was in no doubt that the transplant was the right course of action, but I was very anxious about it and knew it would be challenging.
Self (autologous) and donor (allogeneic) stem cell transplants
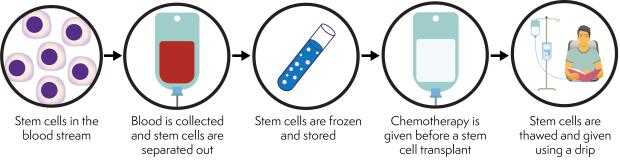
The cells used in a stem cell transplant can be your own stem cells (an ‘autologous’ stem cell transplant) or they can be from someone else (a donor or ‘allogeneic’ stem cell transplant). The key stages of autologous and allogeneic stem cell transplants are summarised below. Stem cell transplants are complicated and each stage involves a number of steps. The entire process can take weeks or months.
In an autologous stem cell transplant, your own stem cells are collected and frozen. You then have high-dose chemotherapy to kill your lymphoma. This also damages the rest of the stem cells in your bone marrow. After the chemotherapy, your stored stem cells are thawed and given back to you. This kind of treatment is sometimes called ‘high-dose therapy and stem cell support’ or ‘high-dose therapy and stem cell rescue’.
In an allogeneic stem cell transplant, the stem cells are collected from a donor. Your transplant team tries to identify a donor whose cells match yours as closely as possible. You have high-dose chemotherapy and you are then given the donor stem cells. As well as helping your bone marrow recover, the donor stem cells develop into new immune cells that recognise your lymphoma cells as foreign or ‘non-self’. This can help your body fight the lymphoma.
Both types of stem cell transplant increase your chance of having a longer-lasting remission from lymphoma. If you need a stem cell transplant, whether you have an autologous or allogeneic transplant depends on your type of lymphoma, your response to treatment and your individual circumstances. Most transplants used to treat lymphoma are autologous.
For more detailed information, see our separate pages on self (autologous) stem cell transplants and donor (allogeneic) stem cell transplants.
Listen to our podcast where John Murray, Nurse Clinician in Bone Marrow Transplant, and Angie Leather, who is Lead Nurse for Transplant and Haematology CNS, talk about the role of stem cell transplants, when they are used and the important differences between autologous (self) and allogeneic (donor) stem cell transplants. This podcast includes discussions around this often very difficult subject, and contains information on side effects and treatment outcomes that may be potentially distressing.
