Adult T-cell leukaemia/lymphoma (ATL)
This information is about adult T-cell leukaemia/lymphoma (ATL), a rare type of T-cell lymphoma associated with the HTLV-1 virus.
On this page
What is ATL?
Adult T-cell leukaemia/lymphoma (ATL or ATLL) is a rare type of non-Hodgkin lymphoma that affects about 1 in 20 people who have a virus called ‘human T-lymphotropic virus type 1’ (HTLV-1). It can be classified as a leukaemia or lymphoma depending on whether the lymphoma affects the blood (leukaemia) and/or lymph nodes (lymphoma). ATL is a type of T-cell lymphoma – a lymphoma that develops from white blood cells called T cells.
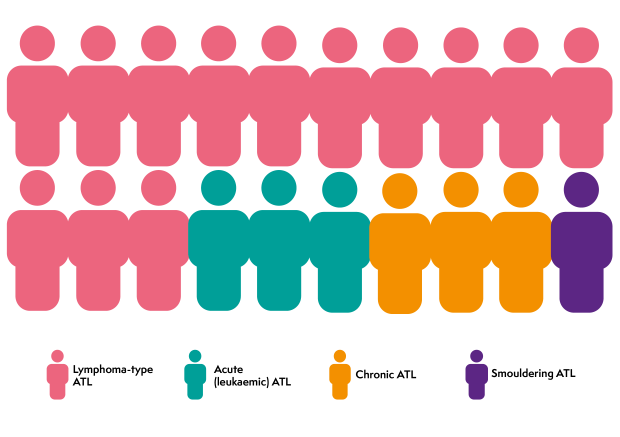
There are four main types of ATL: lymphoma-type ATL, acute (leukaemic) ATL, chronic ATL and smouldering ATL. Low-grade types of ATL can sometimes change (transform) into faster-growing types.
Lymphoma-type ATL
Lymphoma-type ATL is the most common type of ATL. It is a fast-growing (high-grade) lymphoma that accounts for around 13 in every 20 cases of ATL in the UK. It is called ‘lymphoma-type’ because you have abnormal white blood cells in your lymphatic system but not in your blood.
Acute (leukaemic) ATL
Acute (leukaemic) ATL is a fast-growing (high-grade) blood cancer that accounts for around 3 in every 20 cases of ATL in the UK. It is called ‘leukaemic’ because you have lots of abnormal white blood cells (‘leukocytes’) in your blood and your lymphatic system. Acute ATL is more likely to affect other organs, including the nervous system.
Chronic ATL
Chronic ATL is a slow-growing (low-grade) lymphoma that accounts for around 3 in every 20 cases of ATL. It is called ‘chronic’ because it develops slowly over a long time. Chronic ATL affects the blood and the lymph nodes.
Smouldering ATL
Smouldering ATL is a low-grade lymphoma that accounts for around 1 in every 20 cases of ATL. It is called ‘smouldering’ because it can go on for a long time without causing many problems. Smouldering ATL typically affects the skin and occasionally the lungs.
Who gets ATL?
ATL is very rare. Only around 30 people are diagnosed with it in the UK each year. ATL can affect men and women of any age but it most commonly develops around the age of 51.
ATL only affects people who have a virus called ‘human T-lymphotropic virus type 1’ (HTLV-1). HTLV-1 infection is rare in the UK but it is very common in some parts of the world. These include southern Japan, the Caribbean Basin, Central and South America, Iran, Romania and parts of Africa.
HTLV-1 infection is spread from person-to-person through breastfeeding, unprotected sex, sharing contaminated needles or equipment, or infected blood transfusions or organ transplants.
People who have HTLV-1 may not know they are infected. However, only around 1 in 20 people with HTLV-1 develop ATL, often several decades after becoming infected with HTLV-1. Most people with HTLV-1 do not develop lymphoma. Only carriers with a high level of virus in their blood (a ‘high viral load’) are at risk of developing ATL. Your viral load can be measured by a blood test.
ATL can occur within families. It can spread within families through mother-to-child breast feeding. If you have ATL, your brothers and sisters, children and parents should be tested for HTLV-1 infection to monitor their risk.
Symptoms of ATL
The symptoms of ATL depend on the type of ATL you have. The symptoms for lymphoma-type ATL and acute ATL are very similar. The symptoms for chronic ATL and smouldering ATL are also similar.
Symptoms of acute ATL and lymphoma-type ATL
Acute ATL and lymphoma-type ATL are high-grade lymphomas. Symptoms can develop quickly.
The most common symptoms of these types of ATL are:
- swollen lymph nodes
- a swollen liver and spleen, which might make you feel bloated or cause tummy (abdominal) pain
- a skin rash, which can vary from widespread, itchy red patches to lumps or skin tumours that can break down (ulcerate) and scab over
- high levels of calcium in your blood, which can cause sickness, diarrhoea, constipation, headaches, weeing more than usual, or feeling thirsty, weak, tired or confused
- fever, night sweats and weight loss (‘B symptoms’)
- abdominal (tummy) symptoms
- getting more infections than usual, or having difficulty shaking off infections.
Some people with ATL develop skin tumours that grow very quickly. This is sometimes called ‘cutaneous lymphoma-type ATL’. It is treated the same as lymphoma-type ATL but you might need some direct skin treatment, too. This is different from the common types of skin cancer, and is related to the ATL.
In around 1 in 10 people, acute or lymphoma-type ATL can affect your bones, which might make your bones ache or break more easily than normal. Occasionally, ATL can spread to your brain or spinal cord (central nervous system). This tends to be more common in lymphoma-type ATL or acute ATL.
The main difference between the acute and lymphoma-types of ATL is whether or not you have abnormal lymphocytes in your blood:
- The acute form is ‘leukaemic’, which means you have lots of abnormal lymphocytes in your bloodstream.
- In the lymphoma form, you have lots of abnormal lymphocytes in your lymph nodes. They often spread outside your lymphatic system (‘extranodal’ lymphoma) but they don’t affect your blood.
Most people with the acute and lymphoma types of ATL have advanced stage lymphoma (stage 3 or 4) when they are diagnosed.
Symptoms of chronic ATL and smouldering ATL
Chronic and smouldering ATL are low-grade lymphomas. They usually cause mild symptoms.
Smouldering ATL often causes a skin rash but some people don’t have any symptoms at all. You might just have a blood test that shows abnormal T cells in your bloodstream.
The most common symptoms of chronic ATL are:
- a skin rash
- swollen lymph nodes
- a swollen liver or spleen
- high numbers of lymphocytes (a type of white blood cell) in your bloodstream.
These symptoms are usually mild.
Treatment of ATL
ATL is rare in the UK. This makes it difficult to work out which treatments give the best outcome.
The treatment you need for ATL depends what type of ATL you have and how it affects you. We have information on the treatment you might have if you have acute ATL or lymphoma-type ATL, and whether you have chronic ATL or smouldering ATL.
Several targeted drugs are being tested in clinical trials. Your doctor might ask you if you would like to take part in a clinical trial to help test new treatments and to find out what the best treatment is for ATL.
Treatment of acute ATL and lymphoma-type ATL
Acute ATL and lymphoma-type ATL are fast-growing and need to be treated straightaway. It is common for these types of lymphoma to come back (relapse) after treatment.
There is no standard treatment for high-grade ATL. Your doctor might ask you if you would like to take part in a clinical trial to help test new treatments and to find out what the best treatment is for ATL.
If you don’t want to take part in a clinical trial, or if there isn’t one that is suitable for you, you are likely to be treated with strong chemotherapy. Some people also have antiviral drugs such as zidovudine and interferon-alfa to control their HTLV-1 infection. You have blood tests to check for high calcium levels so you can be treated quickly if it develops.
The most common chemotherapy regimens (combination of drugs) used to treat acute or lymphoma-type ATL are:
- CHOP: cyclophosphamide, hydroxydaunorubicin, vincristine (also known as Oncovin®) and prednisolone
- CHEOP: CHOP plus etoposide
- DA-EPOCH: dose-adjusted etoposide, prednisolone, vincristine (also known as Oncovin®), cyclophosphamide and doxorubicin (or hydroxydaunorubicin)
- hyper-CVAD: cyclophosphamide, vincristine, doxorubicin (also known as Adriamycin®) and dexamethasone; ‘hyper’ is short for ‘hyperfractionated’, which means that you have the same drug more than once in a day.
However, your medical team might recommend a different chemotherapy regimen. If you are not fit enough to have strong chemotherapy, you might be treated with lower doses of chemotherapy or gentler options such as oral chemotherapy or antiviral treatment on its own.
If your doctor thinks you are at high risk of your lymphoma affecting your brain and spinal cord (central nervous system or CNS), you might have additional chemotherapy drugs to try to prevent this. You might have these drugs given into a vein (intravenously) or through a lumbar puncture into the fluid around your spinal cord (intrathecal injection). This is called CNS prophylaxis.
If you respond to chemotherapy and you are well enough, your doctor is likely to recommend that you have a donor (allogeneic) stem cell transplant. This gives you a better chance of staying in remission (no evidence of lymphoma). If you don’t respond to chemotherapy, you will switch to a different type of chemotherapy and be considered for a clinical trial if there is one suitable for you.
Treatment of chronic ATL and smouldering ATL
If you have chronic ATL or smouldering ATL and you don’t have any troublesome symptoms, you might not need any treatment at first. Instead, your doctor monitors you closely. This is called active monitoring (‘watch and wait’). It is often used for early stage lymphoma that would not benefit from starting treatment straightaway. However, due to the risk of chronic and smouldering ATL becoming more aggressive, your doctor is likely to offer you treatment. They might ask you if you would like to take part in a clinical trial.
If you don’t want to take part in a clinical trial, or if there isn’t one that is suitable for you, you are likely to be treated with antiviral drugs such as zidovudine and interferon-alfa. These help to fight HTLV-1 infection and slow the growth of ATL.
If you have skin symptoms, you might also have skin-directed (topical) treatments or light therapy.
If your ATL changes to a faster-growing type, continues to get worse even with treatment or you have skin tumours that are growing, you are treated the same way as acute or lymphoma-type ATL.
Relapsed or refractory ATL
It is common for ATL to come back (relapse) after being in remission. Sometimes, ATL doesn’t respond to treatment (refractory lymphoma). In these cases, your doctor might consider:
- a targeted drug, usually through a clinical trial
- a single chemotherapy drug, such as bendamustine or gemcitabine
- a different chemotherapy regimen, such as DHAP, ESHAP, GDP, GEMOX or ICE
- radiotherapy to help treat any symptoms caused by large lumps of lymphoma in a particular area of your body.
Research and targeted treatments
Many targeted drugs are being tested to see if they can help people with T-cell lymphoma. ATL is rare so there are few clinical trials looking specifically at this type of lymphoma. Suitable clinical trials are likely to be recruiting people with several types of T-cell lymphoma. Drugs that are being tested in T-cell lymphomas include:
- antibody treatments such as mogamulizumab, which binds to a protein called CCR4 on abnormal T cells and stimulates the immune system to kill them
- antibody–drug conjugates such as brentuximab vedotin, a strong anti-cancer drug joined to an antibody that binds to a protein called CD30 on the surface of T cells
- immunomodulatory drugs such as lenalidomide, which help your immune system stop the lymphoma cells growing
- checkpoint inhibitors such as avelumab or nivolumab, which help your immune system recognise the lymphoma cells
- epigenetic modifiers (drugs that act on the lymphoma cells and immune cells to restore the immune system to recognise lymphoma cells):
- HDAC inhibitors such as vorinostat, romidepsin or belinostat, which modify your body’s immune response to cancer cells and alter the activity of genes to make cancer cells die
- EZH1/2 inhibitors such as valemtostat, which alters gene expression patterns associated with cancer pathways
- a chemotherapy drug called pralatrexate.
Some of these might be available to you through a clinical trial. If you are interested in taking part in a clinical trial, ask your doctor if there is a trial that might be suitable for you. To find out more about clinical trials or search for a trial that might be suitable for you, visit Lymphoma TrialsLink.
