Lymphoma in young people
This information is about lymphoma in teenagers and young adults (up to 24 years old). We have separate information about lymphoma in children under 15, aimed at parents and carers. If you are over 18, you might also find it useful to read our information on specific types of lymphoma in adults.
There is a lot of information on this page. You might want to read it in chunks. You can use the links under ‘On this page’ to help you navigate to the parts that are most relevant to you.
We also have a page on practicalities if you are a young person with lymphoma.
On this page
Types of lymphoma in young people
We produce a Young person’s guide to lymphoma, which is designed for teens and young adults affected by lymphoma. It covers what lymphoma is, how it is treated, and how to look after yourself during your treatment and beyond. We also produce information in Easy Read format, which uses simple words and illustrations to explain about lymphoma. You can download the books or order printed copies free of charge.
What is lymphoma?
Lymphoma is a type of cancer. It develops when white blood cells called lymphocytes grow in an uncontrolled way. These abnormal lymphocytes build up in your body.
Lymphoma is the most common cancer in teenagers and young adults. It accounts for around 1 in 5 cancers in young people.
Every year in the UK, around 500 young people aged 15 to 24 are diagnosed with lymphoma. Many people have never heard of it before their diagnosis.
If you have lymphoma, it’s not because of anything you did or did not do. You can’t catch lymphoma and you can’t give it to anybody else. In most cases, the cause of lymphoma is not known.
Types of lymphoma in young people
There are lots of types of lymphoma. They are split into two main groups:
Hodgkin lymphoma
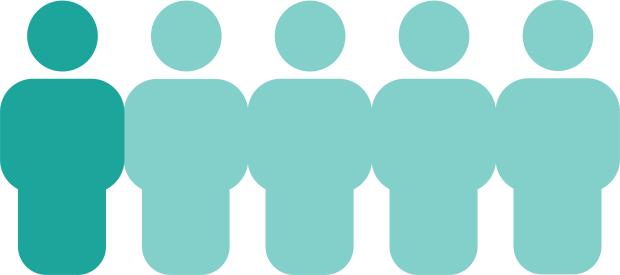
Around 2 in 3 young people diagnosed with lymphoma have Hodgkin lymphoma.
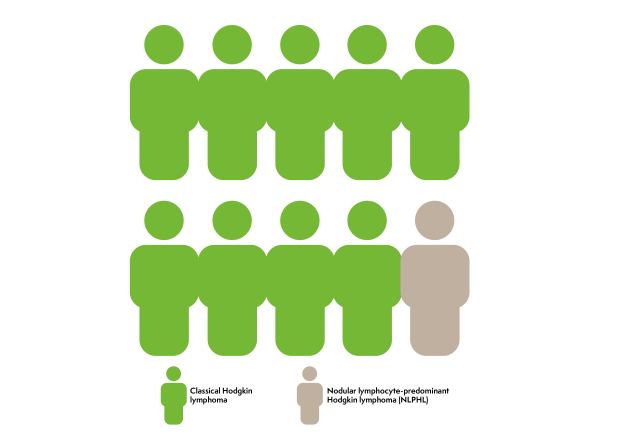
- Most young people have a type called classical Hodgkin lymphoma.
- Up to 1 in 10 young people have a less common type called nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL).
Non-Hodgkin lymphoma
Around 1 in 3 young people diagnosed with lymphoma have non-Hodgkin lymphoma. There are lots of different types of non-Hodgkin lymphoma.
Different types are often grouped together depending on how they behave. Some types of non-Hodgkin lymphoma grow slowly (low-grade lymphomas) and others grow more quickly (high-grade lymphomas). Most non-Hodgkin lymphomas in young people are high-grade. Although this might sound alarming, high-grade lymphomas generally respond very well to treatment and are very likely to go into remission (no evidence of lymphoma) with the right treatment.
The most common types of non-Hodgkin lymphoma in young people are:
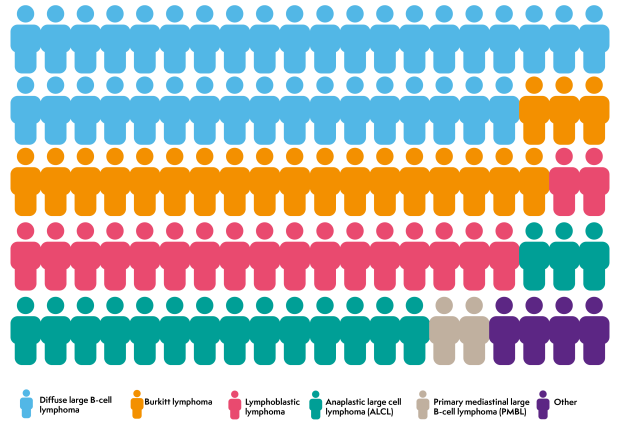
- diffuse large B-cell lymphoma (DLBCL), accounting for 35 to 40 in every 100 cases of non-Hodgkin lymphoma in young people
- Burkitt lymphoma, accounting for around 20 in every 100 cases of non-Hodgkin lymphoma in young people
- lymphoblastic lymphoma, accounting for 15 to 20 in every 100 cases of non-Hodgkin lymphoma in young people
- anaplastic large cell lymphoma (ALCL), accounting for around 20 in every 100 cases of non-Hodgkin lymphoma in young people
- primary mediastinal large B-cell lymphoma (PMBL), accounting for around 2 in every 100 cases of non-Hodgkin lymphoma in young people.
Other types of non-Hodgkin lymphoma are uncommon in young people.
Symptoms of lymphoma in young people
Many of the symptoms of lymphoma can also be symptoms of other illnesses. This can make lymphoma difficult to diagnose.
The symptoms you might experience depend on where the lymphoma is in your body. Symptoms vary from person-to-person even if you have the same type of lymphoma.
In March 2020, I noticed my legs were really itchy and I was having night sweats, but I didn’t think it was anything to worry about. However, I noticed a lump near my collarbone, and it was that which led me to call my GP.
On this page, we cover the most common symptoms of lymphoma in young people:
- swollen lymph nodes
- chest symptoms
- tummy symptoms
- common general symptoms
- low blood counts
- skin symptoms
- brain and nerve symptoms.
You might have some of these symptoms but not others, or you might have different symptoms.
Having any of these symptoms does not necessarily mean you have lymphoma. They are often caused by other, less serious illnesses. If you are worried about your symptoms, contact your GP.
Swollen lymph nodes
The most common symptom of lymphoma in young people is a lump or lumps that don’t go away after a few weeks. These lumps are swollen lymph nodes. Lymph nodes often swell when you have an infection, such as a cold, an ear infection or a sore throat. Swollen lymph nodes caused by infections are usually painful to the touch and go down within 2 or 3 weeks. Swollen lymph nodes caused by lymphoma aren’t usually painful – although, rarely, they might feel painful a few minutes after drinking alcohol. They can grow very quickly and don’t shrink back down.
Swollen lymph nodes often develop in the neck, armpit or groin. You will probably be able to feel these lumps. Some might develop deeper inside your body, where you can’t feel them. These cause different symptoms depending on where they are.
Chest symptoms
If you have lymphoma in your chest, you might wheeze or get out of breath easily, or develop a cough that doesn’t go away. Occasionally, the lymphoma might press on blood vessels in your chest. If this happens, you might get a red, swollen face and the veins in your neck might look more obvious than usual. Hodgkin lymphoma, DLBCL, PMBL and lymphoblastic lymphoma can all develop in the chest.
Tummy symptoms
If you have lymphoma in your tummy (abdomen), you might get tummy pain, sickness, diarrhoea, constipation or a swollen tummy. DLBCL and Burkitt lymphoma often cause tummy symptoms.
Common general symptoms
Lymphoma can cause general symptoms due to the way your body reacts to the lymphoma cells. These include:
- fatigue (extreme tiredness that doesn’t get better with rest)
- drenching sweats, especially at night – these can be so severe that you need to change your nightclothes and bedding
- a high temperature (above 38°C or 100.4°F) that might come and go
- a poor appetite
- losing weight without trying to
- itching.
Night sweats, weight loss and high temperature (fevers) often occur together. They are sometimes called B symptoms. Your doctor will consider whether or not you have B symptoms when they decide on the most appropriate treatment for you.
Low blood counts
If you have lymphoma in your bone marrow (the spongy part of bones where blood cells develop), you might get low blood counts. This will show up on blood tests, but it can also cause symptoms such as:
- tiredness
- shortness of breath
- bruising or bleeding more easily than usual
- picking up infections easily that last longer than usual.
Skin symptoms
If you have lymphoma affecting your skin, you might get a rash or notice dry red patches or scaly lumps on your skin. They might be itchy. ALCL can cause skin symptoms.
Brain and nerve symptoms
Rarely, lymphoma can affect the nerves or brain. This might cause symptoms such as headaches, dizziness or fits (seizures).
Tests for lymphoma
If your GP thinks you might have lymphoma, they will refer you urgently to be assessed by a specialist. You will need tests to find out for certain.
You might have blood tests to start with, to help your doctor find out more about your health. To confirm a diagnosis of lymphoma, though, you will need a small operation called a biopsy. This involves removing a swollen lymph node (or part of one) for testing.
Most young people have a local anaesthetic to have a biopsy. This numbs the area where the sample is being taken so you don’t feel anything. If you need a whole lymph node to be removed, or it is deep inside your body, it might be done under general anaesthetic. This means you are asleep for the whole procedure.
If you have swollen lymph nodes deeper inside your body, you might have an X-ray or scan to help your doctor find the best place to take the biopsy. They usually take the biopsy sample using keyhole surgery.
An expert lymphoma pathologist looks at the biopsy sample under a microscope to find out whether or not it is lymphoma. If it is, they will carry out more lab tests on the sample to find out exactly what type of lymphoma it is.
Staging
If you have lymphoma, you will need more tests to find out how much lymphoma is in your body and exactly where it is. This is called staging. Knowing the stage of your lymphoma helps your specialist plan the best possible treatment for you.
The tests you might have include:
- blood tests to find out how lymphoma is affecting you and to check your general health
- scans such as a PET/CT scan, MRI scan, ultrasound scan or X-ray to see where the lymphoma is in your body
- a bone marrow biopsy to check for lymphoma in your bone marrow (although this is rarely needed nowadays, because it can often be seen on a PET/CT scan instead)
- rarely, a lumbar puncture to check for lymphoma cells in the fluid that surrounds your spinal cord.

You don’t necessarily need all of these tests – your doctor orders the most appropriate tests depending on the type of lymphoma you have and how it is affecting you.
Most people have their tests as an outpatient – they go to hospital for the tests and go home later the same day. You have some of the tests, like the bone marrow biopsy and the lumbar puncture, under an anaesthetic. They might be done at the same time as your biopsy.
Your specialist uses the results of all these tests to work out the stage of your lymphoma. Hodgkin lymphoma in children and young people is staged the same way as in adults. Non-Hodgkin lymphoma is staged slightly differently in children and adults. Young adults with non-Hodgkin lymphoma might be staged using either system. Both systems work out if your lymphoma is ‘early stage’ or ‘advanced stage’. Your medical team might tell you your stage as a number. Stages are numbered from 1 to 4. Stage 1 and 2 are early stage. Stage 3 and 4 are advanced stage.
Because lymphocytes travel all over the body, lymphoma is often advanced stage by the time it is diagnosed. This might sound alarming, but advanced stage lymphoma can be treated very successfully and most young people have a good outlook.
Your specialist should tell you the type and stage of your lymphoma when you have had all your tests. It is important that you know what type of lymphoma you have, so you can find information that is relevant for you.
Outlook
Your lymphoma specialist is the best person to talk to about your outlook, because they know your medical history and all your individual circumstances.
In general, though, treatments for young people with lymphoma are very successful. Most young people who have lymphoma go into complete remission and stay in remission. Complete remission means that tests and scans at the end of treatment show no evidence of lymphoma left in your body.
If you choose to look at survival statistics, remember that they can be confusing. They don’t tell you what your individual outlook is – they only tell you how a group of people with the same diagnosis did over a period of time. Treatments are improving all the time and survival statistics are usually measured over 5 or 10 years after treatment. This means that statistics only tell you how people did in the past. Those people may not have received the same treatment that you will receive. A lot of statistics are very general and include people of all ages. Cure rates in young people are much higher than in older people so the information you find might not be relevant for you. Cancer Research UK has statistics on Hodgkin lymphoma and non-Hodgkin lymphoma if you choose to learn more.
Treatment
Different types of lymphoma need different treatment. Your specialist will work with a team of health professionals (a ‘multidisciplinary team’) to decide on the best option for you. They consider the type of lymphoma you have and how it is affecting you, as well as other factors such as your age and general health.
Helen describes having treatment for primary mediastinal B-cell lymphoma when she was 20
Some young people are treated using options recommended for children with lymphoma. Some young people are treated using options recommended for adults with lymphoma. Your medical team will make a recommendation personal to you, based on your exact circumstances. Your specialist is the best person to talk to about the treatment they recommend. However, in general:
- You are likely to be offered treatment as part of a clinical trial, if there is one suitable for you.
- Most young people have chemotherapy. This might be combined with antibody therapy.
- Some young people have radiotherapy.
There is more about different types of treatment in the sections below.
Most young people are treated at specialist hospitals that have all the facilities they need to diagnose and treat young people with cancer.
Clinical trials
Your specialist might suggest that you have treatment as part of a clinical trial, if there is one suitable for you. Clinical trials are medical research studies involving people. Many young people with cancer take part in clinical trials so that scientists can find better ways to treat them. Clinical trials aim to find out if new treatments, or new ways of using existing treatments, are better than current treatment options. Treatment for lymphoma in young people is generally very successful, so the focus of many trials is to limit side effects, especially in the long-term, while still giving every chance of sending the lymphoma into remission.
If you’re interested in hearing about clinical trials that might be suitable for you, ask your specialist.
Clinical trials are voluntary. If you don’t want to take part, you don’t have to. If you are in a trial but you don’t want to continue with it, you can opt out at any time. In this case, your specialist will give you the best standard treatment instead.
You can find out more about clinical trials, or search for a trial that might be right for you, in our dedicated section, Lymphoma TrialsLink.
Chemotherapy
Chemotherapy means treatment with drugs. Chemotherapy to treat cancer uses drugs that kill cells. Cancer cells usually divide and grow more rapidly than most healthy cells. Chemotherapy works by killing cells that are actively dividing – which is why it is effective at killing cancer cells. However, it can also kill healthy cells that divide rapidly, such as hair root cells, skin cells and blood cells. This is what causes some of the side effects of chemotherapy.
Lots of different chemotherapy drugs are used to treat lymphoma. Usually, several drugs that kill cells in different ways are given together, to kill as many lymphoma cells as possible. Each combination of drugs is known as a chemotherapy regimen. Chemotherapy regimens often have complicated names, such as DA-EPOCH, OEPA, COPDAC or ABVD. These are usually abbreviations of the names of drugs they include.
Watch our chemotherapy animation to find out how chemotherapy works and why it is given in cycles
What chemotherapy will I have?
Lots of different chemotherapy regimens are used to treat lymphoma in young people. Your multidisciplinary team will recommend a chemotherapy regimen based on your individual circumstances. Your specialist will explain which treatment they are recommending, and why they think it is the best choice for you. They will give you information about what to expect and what side effects you might experience.
How long will chemotherapy take?
Chemotherapy is given in cycles. A cycle is a block of chemotherapy followed by some time off treatment to let your body recover. If your body doesn’t recover as quickly as hoped, your next cycle of chemotherapy might be delayed until it is safe for you to have more treatment.
Most young people with lymphoma have several cycles of chemotherapy over several months. You might stay in hospital for some of your treatment and have some as an outpatient. This is when you go into hospital for a few hours at a time to have treatment and come home straight afterwards.
The number of cycles of chemotherapy you need depends on the type and stage of your lymphoma and the exact treatment you are having. Your specialist will tell you how many cycles you are likely to need and how long this will take.
- Young people with Hodgkin lymphoma are likely to have a PET scan after their first few cycles of chemotherapy. The results of the scan are used to decide how many more cycles of chemotherapy you need, and if you need radiotherapy after finishing chemotherapy.
- Treatment for non-Hodgkin lymphoma in young people is sometimes given in phases, using different chemotherapy drugs at different times. Your specialist will tell you what treatment you need at each phase and how long each phase is expected to take. Depending on the type and stage of your lymphoma, your treatment might include:
- Cytoreductive therapy: a short period of treatment to reduce the number of lymphoma cells in your body. This helps prevent some of the side effects of intensive treatments.
- Remission induction: a period of intensive treatment to put the lymphoma into remission.
- Consolidation: a period of less intensive treatment to keep the lymphoma in remission.
- Reinduction: another period of intensive treatment to get rid of any lymphoma cells that might have been left behind.
- Maintenance: a period of gentler treatment to stop the lymphoma coming back.
I started treatment with ABVD chemotherapy. A scan showed that the lymphoma had halved, but they wanted to move on to more intensive chemotherapy, so my chemotherapy was changed to BEACOPPesc. My doctor also explained that I would need radiotherapy at the end of chemotherapy to get rid of the last traces of the lymphoma.
How will I have chemotherapy?
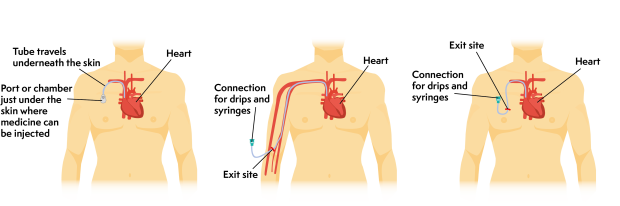
Many chemotherapy drugs are given through a drip into a vein (intravenously). This can be through a cannula, which is a soft tube that is put into a vein – often in your hand or forearm – using a needle. Cannulas need to be taken out and replaced between treatments. Many people have a central line fitted instead, so they don’t need to have a needle every time they need treatment. A central line can also be used to take blood samples for blood tests.
A central line is a thin, soft tube that goes underneath the skin and into one of the main veins leading into your heart. It is put in place under general anaesthetic. Once in place, it usually stays in for the whole of your treatment. Your medical team will tell you how to look after the line at home. It is taken out at the end of treatment.
There are different types of central line, depending on exactly how and where they are put in.
You might also have some drugs by mouth. This could be tablets, capsules, or syrup.
Some young people with non-Hodgkin lymphoma might also need chemotherapy given directly into the fluid around the spinal cord. This is called intrathecal chemotherapy. It is given through a thin needle in the lower back (a lumbar puncture). Intrathecal chemotherapy helps stop lymphoma spreading to the brain or spinal cord. Not all young people need intrathecal chemotherapy.
You are monitored closely throughout treatment. Your specialist checks how much lymphoma has been killed and how well you are coping with the treatment.
Radiotherapy
Radiotherapy uses powerful X-rays to kill lymphoma cells. It is not often used to treat young people with non-Hodgkin lymphoma. Some young people with Hodgkin lymphoma might have radiotherapy if they have some lymphoma left in their body after their first two cycles of chemotherapy. In this case, it is given after you finish your chemotherapy.
Radiotherapy is given every week day for a few days or weeks, usually as an outpatient.. Each treatment only lasts a few minutes but it can take a while to position the X-ray beam so it focuses precisely on areas affected by lymphoma. This reduces the effect of radiotherapy on healthy cells. You have ink marks or tiny tattoos put on your skin to make sure the same area is treated every time.
The lowest possible dose of X-rays is used to reduce the risk of damaging growing bones and muscles or harming organs. It also lowers the chance of late effects (side effects that develop long after treatment has finished).
The type of radiotherapy used in lymphoma treatment doesn’t make you radioactive. You can still be close to other people when you have had radiotherapy.
Targeted treatments and antibody therapies
Targeted treatments are medicines that have been specially designed to attack particular proteins or chemical signalling pathways in lymphoma cells. They attack lymphoma cells more precisely than chemotherapy. This means they are able to kill lymphoma cells with fewer unwanted effects on healthy cells. Some of these treatments are only licensed for adults with lymphoma. They might be available for under 18s through clinical trials.
- Nivolumab and pembrolizumab are targeted treatments that block the proteins lymphoma cells use to turn off your immune cells. They are used for some people with Hodgkin lymphoma that has come back or didn’t respond to previous treatments. You have them through a drip or central line.
- CAR T-cell therapy is a targeted treatment that takes cells from your own immune system, called T cells, and modifies them in a lab to recognise and kill lymphoma cells. It is used for some people with DLBCL or PMBL that has come back or didn’t respond to previous treatments.
Antibody therapy is a type of targeted treatment. It uses antibodies that have been specially made in a lab to stick to a protein on a cancer cell. This activates the immune system to destroy the cancer cell.
- Rituximab is an antibody therapy that can be used to treat Burkitt lymphoma and DLBCL in young people. You have it through a drip or central line, in combination with chemotherapy. You have pre-medication first, to help prevent any reactions. You have your first dose very slowly, so your specialist can check for any reactions.
- Brentuximab vedotin is an antibody joined to a chemotherapy drug. It delivers the drug directly to the lymphoma cells. It is used for some people with Hodgkin lymphoma or ALCL that has come back or didn’t respond to previous treatments. You have it through a drip or central line, on its own or in combination with chemotherapy. You might have pre-medication first, to help prevent any reactions.
- Polatuzumab vedotin is another antibody joined to a chemotherapy drug. It is used for some people with DLBCL that has come back or didn’t respond to previous treatments. You have it through a drip or central line, in combination with chemotherapy. You have pre-medication first, to help prevent any reactions.
Side effects of treatment
Treatment aims to kill lymphoma cells, but it can also damage some of your healthy cells. This can cause unwanted effects on your body, known as side effects.
For my own mental sanity, I weirdly wanted to be ill. I needed the confirmation that the drugs were working.
Most side effects are short-term but some of them can be longer lasting.
Everyone responds differently to treatment, so it is difficult to predict exactly what side effects you might get. Your medical team will tell you about side effects that might happen with the particular treatment they recommend for you, and will monitor you carefully for them.
Side effects that commonly occur during treatment for lymphoma include:
- feeling sick or being sick
- hair loss
- low blood counts:
- a low level of neutrophils, a type of white blood cell that helps fight infections, increases your risk of getting infections
- a low level of red blood cells, which carry oxygen around your body, can make you feel tired or short of breath
- a low level of platelets, which help your blood clot, can make you bruise more easily than usual or bleed longer after a minor injury
- sore mouth and throat
- weight loss or weight gain.
Some treatments for lymphoma might affect your fertility in the future. Your specialist should tell you if this is likely to be the case. If it is, they will talk to you about options you might wish to consider to help preserve your fertility.
Tell your medical team if you have any side effects, however minor they seem. There are effective treatments for many side effects. Your medical team can also advise you on things you can do yourself to help you cope with your treatment.
What happens if lymphoma comes back or doesn’t respond to treatment?
Most young people with lymphoma are treated successfully and stay in remission.
Occasionally, lymphoma may not respond to treatment as well as expected (refractory lymphoma), or comes back (relapses) after treatment. If this happens, your specialist will suggest different treatment options.
You might be offered treatment as part of a clinical trial. If there isn’t a clinical trial suitable for you, or if you don’t want to take part in one, your specialist will recommend the best available treatment for you. The treatment you might have depends on your age and your type of lymphoma. It might include:
- a different combination of chemotherapy drugs (sometimes given with radiotherapy)
- high-dose chemotherapy followed by a stem cell transplant
- a targeted treatment such as pembrolizumab or nivolumab
- antibody therapy such as brentuximab vedotin or polatuzumab vedotin
- CAR T-cell therapy.
After treatment

Having lymphoma has changed my perspective on life. I really treasure things that come my way. A teenage cancer diagnosis has made me more socially aware and keener to get involved with fundraising and giving back to society.
During and at the end of your treatment, you have tests and scans to check how well you have responded. If these tests and scans show no evidence of lymphoma, it is called remission. Once treatment is finished and you are in remission, you have follow-up appointments at the clinic for many years. These are to check that:
- You are recovering well from treatment.
- You are growing and developing well.
- There are no signs of your lymphoma coming back. The risk of this happening gets much lower over time.
- You are not developing any late effects from your treatments (side effects that can develop months or years later).
The few months that follow a lymphoma diagnosis can be very difficult, and it can take time after your recovery to come to terms with what has happened. Many people struggle with their feelings at this time. It is natural to need a period of adjustment while you try to move forward with life after lymphoma.
There are many ways that you can get support, both emotional and practical. You might find it helpful to read our information on practicalities if you are a young person with lymphoma, which includes tips on looking after yourself and taking care of your wellbeing.
Late effects
Most young people who are treated for lymphoma recover well with few long-term effects. However, because you have had cancer treatment, you have a higher risk of developing certain health problems in later life than people who haven’t. These are called late effects. They can develop months or years after treatment for lymphoma. They include:
- fertility problems
- effects on your growth, if you are still growing
- other cancers later in life
- heart disease
- lung problems
- hormone problems.
Your specialist will monitor you carefully for late effects at your follow-up appointments. They should also tell you any signs or symptoms to look out for. Make sure you go to any screening tests you are invited to attend (for example, breast cancer screening). Detecting late effects early can limit the problems they cause.
