Classical Hodgkin lymphoma
This information is about classical Hodgkin lymphoma and its treatment. We have a separate page about nodular lymphocyte predominant Hodgkin lymphoma, a rare type of Hodgkin lymphoma that needs different treatment.
On this page
What is classical Hodgkin lymphoma?
What is classical Hodgkin lymphoma?
Lymphoma is a type of blood cancer that develops when white blood cells called lymphocytes grow out of control. Lymphocytes are part of your immune system. They travel around your body in your lymphatic system, helping you fight infections.
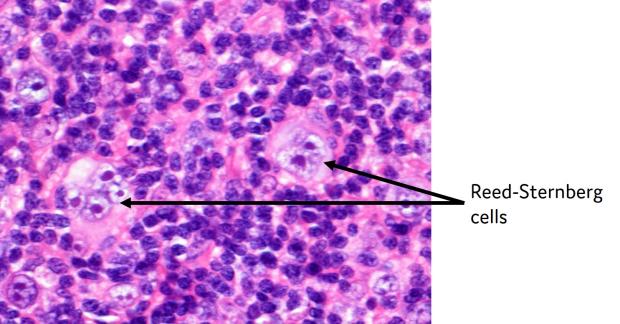
There are lots of different types of lymphoma. Classical Hodgkin lymphoma is a particular type that contains abnormal cells called Reed–Sternberg cells. Doctors can see these cells when they look at biopsy samples of classical Hodgkin lymphoma under a microscope.
There are four subtypes of classical Hodgkin lymphoma. They are named after the appearance of the lymphoma cells and the cells surrounding them.
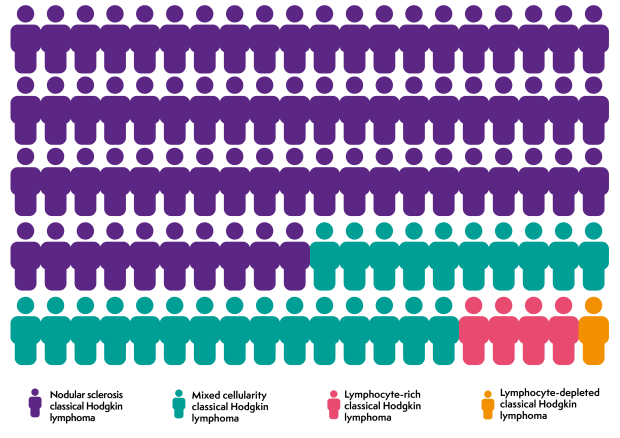
Nodular sclerosis classical Hodgkin lymphoma is more common in young adults. Mixed cellularity classical Hodgkin lymphoma is more common in older adults.
All the subtypes of classical Hodgkin lymphoma are diagnosed and treated in the same way.
Who gets classical Hodgkin lymphoma?
Around 2,000 people develop classical Hodgkin lymphoma each year in the UK. It can develop at any age, but most people diagnosed are between the ages of 15 and 34, or over 60. We have separate information on lymphoma in children (aged 0 to 15) and lymphoma in young people (aged 16 to 24).
Classical Hodgkin lymphoma affects slightly more males than females. It can affect people of any ethnic background.
Scientists don’t know exactly what causes classical Hodgkin lymphoma. Lots of different factors are likely to be involved
About 40 out of 100 cases of Hodgkin lymphoma are related to a past infection with the Epstein-Barr virus (EBV). EBV is a very common virus that can cause glandular fever. EBV infects B lymphocytes. About 9 in 10 adults have been infected with EBV but many people don’t know they’ve had it because it might not cause any symptoms. After you’ve been infected with it, EBV stays in your body but it is normally kept under control by your immune system.
People who have been infected with EBV have a higher risk of developing Hodgkin lymphoma than people who haven’t, with the highest risk being at around 4 years after EBV infection. However, most people who have had EBV do not get Hodgkin lymphoma. Scientists don’t know why some people who have had EBV get lymphoma while most don’t.
Other things that increase your risk of developing classical Hodgkin lymphoma include:
- having a lowered immune system
- family history: lymphoma is not passed down from parents to children (inherited), but you have a very slightly higher risk of developing lymphoma if you have a close relative who has it.
Symptoms of classical Hodgkin lymphoma
The most common symptom of classical Hodgkin lymphoma is a lump or lumps that don’t go down after a couple of weeks. These are swollen lymph nodes. They are usually painless and feel rubbery when you touch them. They are most often found in the neck or just above the collar bones. They can also develop in other parts of your body, such as your armpits or groin.
Many people with classical Hodgkin lymphoma have swollen lymph nodes inside their chest. This might make you cough or feel breathless, or it might not cause any symptoms at all. Occasionally, people with Hodgkin lymphoma have swollen lymph nodes that become painful a few minutes after drinking alcohol. This symptom is unusual – fewer than 1 in 20 people with Hodgkin lymphoma experience it – but it is a strong sign of Hodgkin lymphoma.
It is important to remember that lymph nodes can swell for lots of reasons. Most people with swollen lymph nodes do not have lymphoma.
I had been gradually losing weight, and I’d had a couple of infections needing antibiotics. I put those down to stress, but then I felt a hard lump on my neck just above my collar bone. This definitely set the alarm bells ringing, but the final straw came when I started to feel pain in my chest whenever I took a deep breath.
Around 1 in 4 people with Hodgkin lymphoma have symptoms known as 'B symptoms'. These are:
- fevers (temperature above 38ºC)
- drenching sweats, especially at night
- unexplained weight loss.
Whether or not you have B symptoms can affect which treatment options are most appropriate for you.
Some people have other symptoms, such as itching or fatigue. Rarely, Hodgkin lymphoma starts in an organ in your body rather than a lymph node. The symptoms depend on which part of your body is affected.
Diagnosis and staging of classical Hodgkin lymphoma
Hodgkin lymphoma is diagnosed through a small procedure called a biopsy. This involves removing a swollen lymph node, or a sample of cells from it. It is usually done under local anaesthetic. An expert lymphoma pathologist examines the sample under a microscope and does specialised tests on it to find out what type of lymphoma it is.
On 16 September Jo went for a repeat ultrasound of the lump in his neck. As there was no change in the lump, the sonographer recommended a biopsy and just over a week later we attended a haematology appointment. The biopsy revealed that Jo had Hodgkin lymphoma.
If you are diagnosed with Hodgkin lymphoma, you need other tests to find out which areas of your body are affected. This is called staging. Most people have lymphoma staged by having a PET/CT scan. Some people, particularly children, might have an MRI scan.
You also have blood tests to:
- look at your general health
- check your blood cell counts
- make sure your kidneys and liver are working well
- rule out infections that could flare up when you have treatment.
Rarely, you might have a test to remove a sample of bone marrow (a bone marrow biopsy), to check if you have lymphoma cells in your bone marrow.
You usually have these tests as an outpatient. It takes a few weeks to get all the results.
Waiting for the results of your tests can be a worrying time. However, it’s important for your medical team to know exactly what type of lymphoma you have and how it is affecting you. This helps them plan the most appropriate treatment for you.
Outlook for classical Hodgkin lymphoma
Classical Hodgkin lymphoma generally responds very well to treatment. Most people are cured, even if their lymphoma is advanced when it is diagnosed.
Your lymphoma specialist is the best person to talk to about the likely outcome of your treatment. They can use the results of your tests and other factors (such as your age, any other conditions you have and how fit you are) to help them judge how likely you are to respond to a particular treatment.
When I was told I was in remission, I remember feeling euphoric. I was very excited the whole day. But very soon afterwards I felt numb – and then I felt bad for feeling that way. You’re trying to adjust to the emotional impact of being ill, then being in remission, and it’s really hard. You experience such a range of emotions and it all feels a little like a dream.
Watch Andy talk about his diagnosis of Hodgkin lymphoma and how he kept positive through treatment
This video was produced when Lymphoma Action was called the Lymphoma Association.
Treatment for classical Hodgkin lymphoma
Treatment for classical Hodgkin lymphoma usually involves chemotherapy, sometimes followed by radiotherapy.
The exact treatment you need depends on the stage of your disease and how it is affecting you. Your medical team are likely to consider different treatment options depending on whether you have early disease (stage 1 or stage 2), more advanced disease (stage 3 or stage 4) or if you are over 60. They also consider factors such as:
- your general health and fitness
- your feelings about treatment
- other factors that might be important to you in the future, such as having a family
- any potential side effects, long-term or late effects (health problems that develop months or years after treatment) of the treatment.
Your medical team should explain the possible side effects and late effects of your planned treatment.
The most common chemotherapy regimens (combinations of chemotherapy drugs) used to treat Hodgkin lymphoma are called ABVD and escBEACOPDac.
- ABVD is doxorubicin (also known as Adriamycin®), bleomycin, vinblastine and dacarbazine. You usually have all these drugs every 2 weeks through a drip into a vein. The 2-week break allows your body to recover between treatments. Each 4 weeks of treatment is called a ‘cycle’.
- escBEACOPDac is an escalated dose of bleomycin, etoposide, doxorubicin (also known as Adriamycin®), cyclophosphamide, vincristine (also known as Oncovin®), prednisolone and dacarbazine. You have all these drugs every 2 or 3 weeks. You have most of them through a drip into a vein. You have procarbazine and prednisolone as capsules or tablets that you take by mouth. escBEACOPDac is more effective at curing Hodgkin lymphoma but is more likely to have both short-term and long-term side effects.
You might have a PET/CT scan after your first few cycles of treatment to check how well you are responding. Your consultant uses the results of the scan to decide how many more cycles of treatment you need, whether you should change to a different chemotherapy regimen and whether radiotherapy might be appropriate for you.
Treatment for early stage classical Hodgkin lymphoma
For early stage classical Hodgkin lymphoma, your doctor considers the signs and symptoms you have before deciding what chemotherapy is most likely to be effective for you and how long you should be treated for. These are sometimes called ‘prognostic indicators’. They include:
- whether you have very enlarged lymph nodes in your chest, or enlarged lymph nodes in several areas of your body
- whether you have B symptoms
- whether your blood tests show you have a high level of inflammation
- how old you are
- whether you have any lymphoma outside your lymphatic system (extranodal disease).
You may be told you have ‘early favourable’ or ‘early unfavourable’ Hodgkin lymphoma based on these factors. People with early favourable disease may need slightly less treatment, but early unfavourable is still highly curable.
If you don’t have any of these signs, you are most likely to be treated with two to three cycles of ABVD followed by radiotherapy.
If you do have any of these signs, the most likely treatments are:
- Four cycles of ABVD followed by radiotherapy.
- Two cycles of ABVD followed by four cycles of AVD. If your interim PET/CT scan shows no evidence of lymphoma, radiotherapy isn’t usually given, although some people may have it.
- Two cycles of escBEACOPDac and two cycles of ABVD. No radiotherapy is given after this.
You might not need radiotherapy if:
- you do not have any B symptoms
- you do not have any lumps of lymphoma bigger than around 10cm
- a PET/CT scan shows all your lymphoma has gone after chemotherapy
- you are a young female and radiotherapy might affect your breast tissue.
Chemotherapy without radiotherapy is less likely to cause long-term side effects, but you have a slightly higher risk of your lymphoma coming back (relapsing). If you don’t have radiotherapy, you usually have between three and six cycles of chemotherapy. Your doctor should discuss the treatment choices with you and take your views and wishes into account.
I started treatment with ABVD chemotherapy. The first session knocked me off my feet and I felt tired and emotional. A scan showed that the lymphoma had halved, but they wanted to move on to more intensive chemotherapy, so my chemotherapy regimen was changed to BEACOPPesc. My doctor also explained that I would need radiotherapy at the end of chemotherapy to get rid of the last traces of the lymphoma.
Treatment for advanced stage classical Hodgkin lymphoma
Advanced stage classical Hodgkin lymphoma is also usually treated with chemotherapy, but you are likely to have more cycles of treatment. The most commonly used treatments are six cycles of ABVD or four to six cycles of escBEACOPDac. Your consultant will discuss the treatment options with you.
You will probably have a PET/CT scan after your first few treatment cycles. Depending on the results of your scan, your doctor might recommend changing to a different chemotherapy regimen or adjusting the number of cycles or chemotherapy drugs you need. For example, if there is no evidence of lymphoma on a PET/CT scan after two cycles of treatment, you might not need the bleomycin component of your chemotherapy (the ‘B’ of ABVD or escBEACOPDac) for the rest of your treatment cycles.
Alternatively, if you are on escBEACOPDac, you might only need another two cycles of treatment rather than four.
You might also have radiotherapy if there are any lumps of lymphoma left after your chemotherapy. Most people with advanced stage classical Hodgkin lymphoma do not have radiotherapy.
My life slowed down to just concentrating on getting through each moment; drug to drug, endless exams, needles, biopsies and tubes. The cure seemed to be as dangerous as the disease. A meditative focus on the small things that mattered really helped. I found a great deal of comfort in talking to those in hospital who had had similar experiences and spending time with family and friends.
Treatment for people over 60
About 1 in 5 people diagnosed with Hodgkin lymphoma are over 60. People over 60 are generally more likely to experience serious side effects than younger people. Your doctor will consider your fitness and any other health problems you have. They might recommend a less intensive treatment if they think you have a higher risk of experiencing side effects. They always aim to give you a treatment that is as safe and effective as possible with the lowest possible risk of causing side effects. Radiotherapy is more frequently used in older people as late effects are a less important consideration.
ABVD can be given to people over 60. However other chemotherapy regimens are used more often in this age group, such as:
- ChlVPP: chlorambucil, vinblastine, procarbazine and prednisolone. You have vinblastine through a drip into a vein. You have the other drugs as tablets or capsules that you take by mouth. Each treatment cycle is 28 days.
- AVD: doxorubicin (also known as Adriamycin®), vinblastine and dacarbazine. Each treatment cycle is 28 days and is given through a drip into a vein.
Follow-up of classical Hodgkin lymphoma
I had follow-up checks every three months, then six months, then annually. The advice at the sessions slowly changed from checks to make sure I was clear of the original problems, to longer-term health advice. This included staying fit and eating healthily.
When you are in remission after treatment, you have follow-up appointments to check that:
- you are recovering well from treatment
- you have no signs of the lymphoma coming back (relapsing)
- you are not developing any late effects.
At these appointments, your doctor examines you and asks if you have any concerns or symptoms. You might have blood tests. You are unlikely to have a scan unless you have troubling symptoms.
Most hospital teams offer follow-up in their clinic for at least 2 years after treatment for Hodgkin lymphoma. Some hospitals offer follow-up for 5 years or longer. You might have regular follow-up appointments, or you might be given guidance on booking your own appointments as-and-when you need them.
After your follow-up period ends, your GP usually becomes your main point of contact if you have any concerns or notice anything unusual. Your GP should have a record of your diagnosis and all the treatment you’ve had.
Relapsed and refractory classical Hodgkin lymphoma
In a small number of people, classical Hodgkin lymphoma does not respond to initial treatment (refractory lymphoma) or comes back (relapses) after successful treatment. In either case, there are other treatment options that your doctor can suggest.
If the lymphoma is only in one place in your body, you might be given radiotherapy to the affected area.
If your Hodgkin lymphoma has not responded to treatment, or has come back, you might have more chemotherapy. This is likely to be a different combination of drugs from the ones you had first time round. It is sometimes called ‘salvage’ chemotherapy. Lots of different chemotherapy drugs are used for salvage chemotherapy. The exact ones you have depends on lots of factors, including:
- the stage of your lymphoma
- how old you are
- whether you have any other illnesses
- what side effects you experienced with your previous treatment.
If you respond to salvage chemotherapy and you are fit enough, your doctor might recommend a stem cell transplant. This involves having very high-dose chemotherapy with previously collected stem cells supporting your body through it. It is a very intensive treatment. You need tests beforehand to make sure you are fit enough to have it. We have separate information about stem cell transplants and what they involve.
You might need different treatment if:
- you do not respond to salvage chemotherapy
- you are not fit enough to have a stem cell transplant
- your lymphoma comes back after a stem cell transplant.
If this is the case, you might be offered a different combination of chemotherapy drugs, or a targeted treatment such as:
Research in classical Hodgkin lymphoma
Treatment for classical Hodgkin lymphoma is usually successful but doctors continue to research treatments that might provide better outcomes. They aim to find treatments that are effective with as few side effects and late effects as possible. Some research is looking at how to predict who will respond to which treatments, or who will need radiotherapy after chemotherapy and who won’t.
Your medical team might offer you the chance to take part in a clinical trial, if there is one suitable for you. You can find out more about clinical trials and search for a trial that might be suitable for you at Lymphoma TrialsLink.
