Having a stem cell transplant
Stem cell transplants are an intensive form of treatment that involve a number of different steps. This page outlines the main steps in self (autologous) and donor (allogeneic) stem cell transplants.
On this page
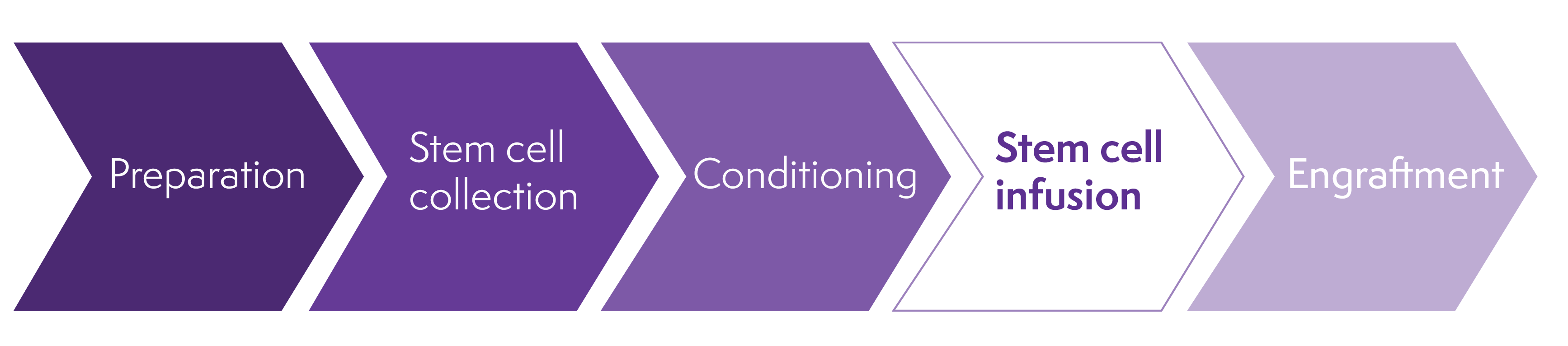
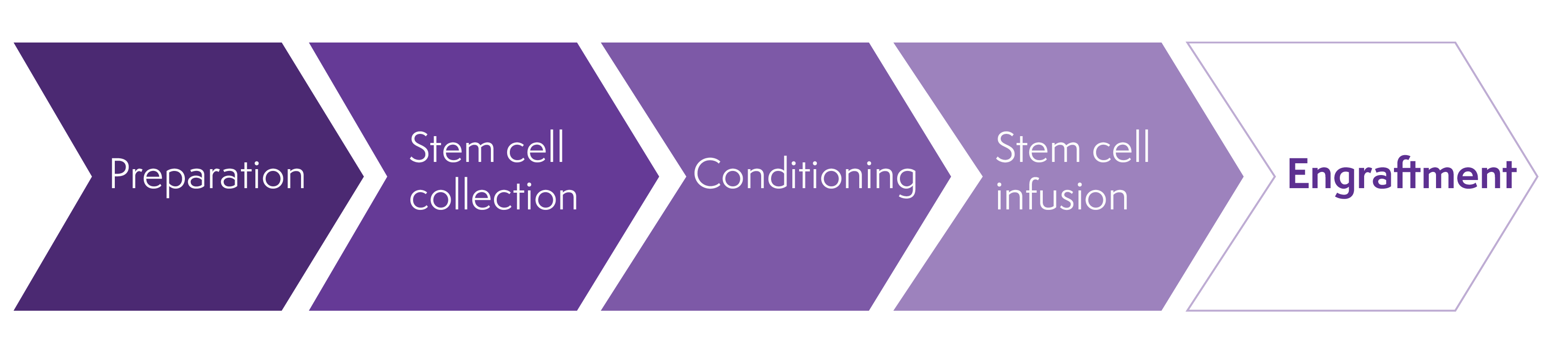
Stages of a stem cell transplant
High-dose anti-cancer therapy (conditioning)
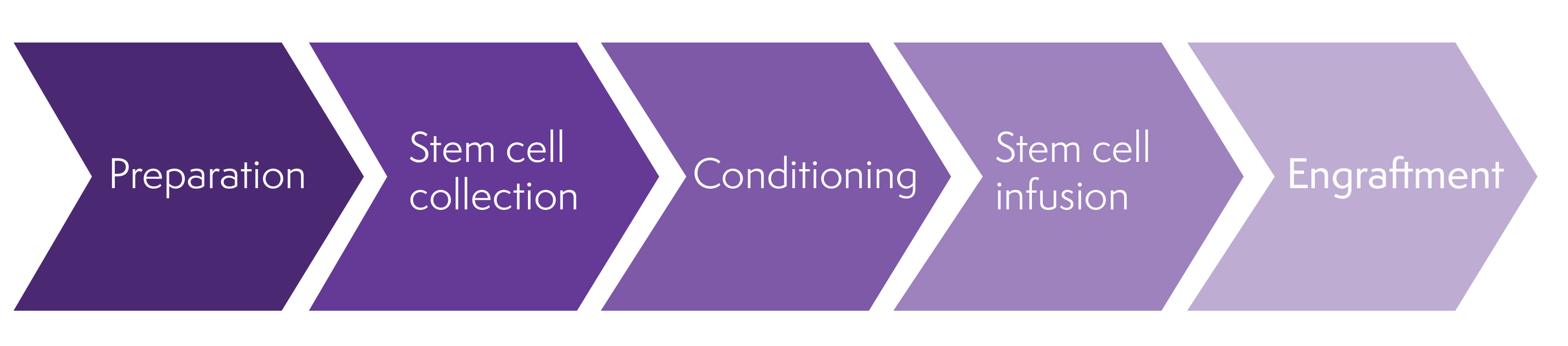
Stages of a stem cell transplant
Stem cell transplants need a lot of preparation and recovery takes many months. It can help to think of the process in stages:
Preparation
Depending on the type of lymphoma you have and how well it has responded to treatment, you might need chemotherapy before you can be considered for a stem cell transplant. This is sometimes called ‘salvage therapy’ or ‘remission induction’. It aims to reduce your lymphoma as much as possible to give you the best chance of responding to a stem cell transplant. If you need salvage therapy, your medical team tells you what chemotherapy regimen is the best option for you and how long you have it for. They will assess how well you respond to the salvage therapy before planning your stem cell transplant. Salvage therapy is not the same as the high-dose conditioning therapy you have as part of your transplant.
The weeks and months before your stem cell transplant involve lots of appointments, tests and scans to prepare for your transplant. Only certain treatment centres carry out stem cell transplants so you might be referred to a different hospital. There are around 50 transplant centres in the UK. Your transplant coordinator (usually a clinical nurse specialist) is your key contact during your preparation for a transplant.
- Your medical team talks to you about what a stem cell transplant involves and what the risks and benefits might be for you. They explain about the possible side effects and complications. They tell you how long you are likely to stay in hospital, what care you might need afterwards and how you are followed-up. There can be a lot of information to take in. Ask as many questions as you want to make sure you understand everything. You might find it helpful to take a notepad to write down any information you are told and any questions you want to ask.
- You have tests to make sure you are well enough to have the transplant. These include blood tests to find out how well your liver and kidneys are working and to check if you have any viruses that might flare up when your immune system is low after your transplant. You have scans and other tests to check how well your heart and lungs are working.
- You might be asked to have a dental check-up to rule out any underlying infections.
- If you are having a donor (allogeneic) stem cell transplant, you have further blood tests to allow your medical team to find a suitable stem cell donor.
- You might also have tests and scans to check on your lymphoma, such as a PET/CT scan to check on your lymphoma status.
- You have a central line (or central venous catheter) fitted. This might be a ‘PICC’ line, a ‘Hickman®’ line or a ‘Groshong®’ line. They are all thin plastic tubes that are inserted into a large vein in your arm or upper chest. They can stay in place for several months. Central lines make it easier for your medical team to give you drugs directly into your veins (intravenously). Your medical team give you information on how to look after your line.
Planning ahead
Most people stay in hospital for a few weeks to have a stem cell transplant. Some transplant centres offer day care (also called ‘ambulatory care’) for people who are well enough and who have a relative or close friend who is able to be with them at all times. This means you stay at home – or, if you live far away from the hospital, at accommodation arranged by your transplant centre. You travel to hospital every day for treatment, blood tests and check-ups but you go home (or to your arranged accommodation) at night. You can contact your transplant centre at any time of the day or night if you need to. If necessary, you can be admitted to hospital.
Whether you have your stem cell transplant as a hospital inpatient or in ambulatory care, you need close follow-up afterwards. Many people do not feel well enough to return to work for several months after a stem cell transplant. For some people, it can take up to a year to recover. You may be eligible for financial support during this time.
Before your transplant, it is a good idea to plan the practical aspects of your life, such as work, home life, childcare (if necessary) and transport to-and-from appointments.
Think about the support you might need during your treatment and recovery. Your medical team can advise you on any support available to you.
If you are having your stem cell transplant in hospital, think about what you need to take in with you. Your hospital should be able to advise you on this. You might want to take:
- soft, comfortable clothes and pyjamas
- gentle toiletries and moisturisers and a toothbrush with very soft bristles
- soft toilet roll or moist wipes
- things to pass the time, such as books, audiobooks, games, your tablet, phone or laptop
- things to brighten up your hospital room
- if your hospital allows it, your own soft towels and bedding (as long as you have somebody who can wash them regularly for you).
Stem cell transplants can be difficult to cope with emotionally and psychologically. You might be offered psychological support or counselling before or during your transplant to help you prepare and cope with the process.
You might find it useful to talk to someone who has had a similar diagnosis, treatment or transplant to you. You can ask your CNS/ transplant coordinator who should be able to introduce you to a suitable person. You can also ask about being put in touch with a Lymphoma Action Buddy, someone who has been through a similar experience to you.
Talk to people, don’t be afraid to talk to people; they are part of this whirlwind that is lymphoma. They can help you think through decisions now and in the future.
The treatment involved in stem cell transplants could reduce your fertility. Your medical team can tell you if this is likely to affect you. If your fertility is likely to be affected and you think you might want to start a family in the future, talk to your medical team. They can refer you to a specialist to discuss options for preserving your fertility before you start your treatment.
Collecting the stem cells
The process of collecting stem cells depends on whether you are having a stem cell transplant using your own cells, or using donor cells.
Collecting stem cells for a self (autologous) stem cell transplant
You may want to skip this section if you are having a donor (allogeneic) stem cell transplant.
If you are having a stem cell transplant using your own stem cells, the cells are collected from your bloodstream. Before this happens, you need treatment to move the stem cells from your bone marrow to your bloodstream. This is sometimes called ‘mobilisation’.
You have medicine to help mobilise your stem cells. This might be growth factors on their own, or growth factors combined with chemotherapy. The chemotherapy might be part of your salvage treatment (if you need it) so you don’t have any extra chemotherapy drugs.
To mobilise your stem cells, you have daily injections of a growth factor called G-CSF. Growth factor stimulates production of stem cells in your bone marrow and helps the stem cells move into your bloodstream. Depending on what other treatment you are having, you might not need to go to hospital for the injections. Your medical team can show you, or someone else, how to do them at home, or can arrange for a nurse to do them for you.
You usually have growth factor injections for 4 to 7 days. You have regular blood tests to see how your blood counts are responding.
The most common side effects of G-CSF are a high temperature, muscle and bone aches and pains, and feeling or being sick. These symptoms can be caused by other things, including serious conditions such as neutropenic sepsis, so tell your medical team if you experience them. You might find paracetamol helpful if you have pain, but you may need something stronger. Your medical team can advise you which pain relief medications are suitable for you and can give you more information about any other side effects you might experience.
When you have enough stem cells in your bloodstream, they are collected using a machine called a ‘cell separator’. This is called ‘apheresis’ or ‘stem cell harvest’. A doctor or nurse puts thin, flexible, plastic tubes into a vein in each of your arms (or they might use your central line, if you have one fitted). They connect these tubes to the cell separator machine. Your blood is taken from a tube in one arm and passes through the machine. The machine collects the stem cells and returns the rest of your blood into your other arm. This process takes a few hours. You have to keep your arm still during this process and cannot move around much.
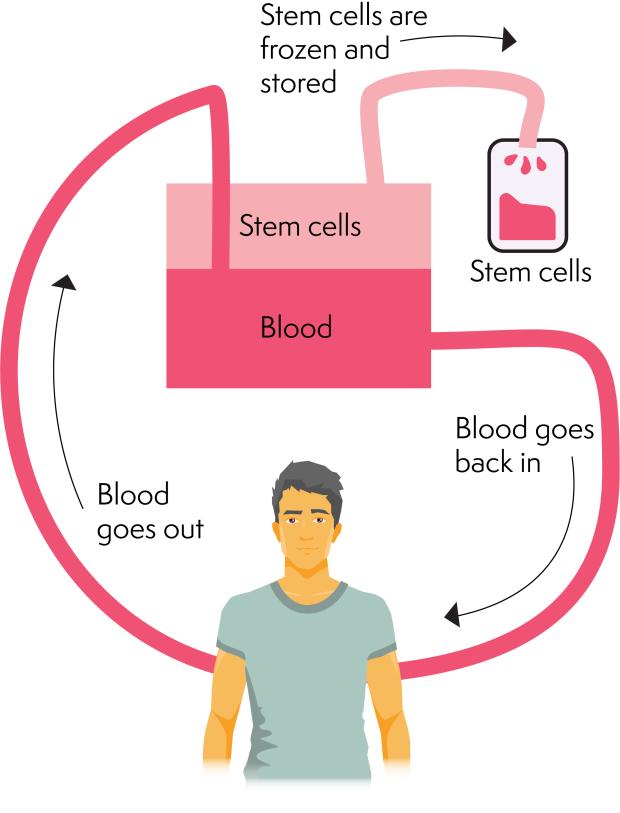
The stem cells are measured, frozen and stored ready to be thawed and given back to you on the day of your transplant.
If not enough stem cells are collected, you might need another day or two of G-CSF injections before having your stem cells collected again. You might also be given a drug called plerixafor (also known as Mozobil®), which blocks a protein on the surface of stem cells that normally keeps them in the bone marrow. Blocking this protein helps stem cells be released into the blood.
It can take up to four stem cell harvests to collect enough stem cells for a transplant.
Some people do not have enough stem cells collected from their blood for a stem cell transplant. If this is the case for you, your doctor will discuss your options with you. Rarely, it might be possible to collect stem cells directly from your bone marrow, or you might be able to have a stem cell transplant using donor cells (an allogeneic stem cell transplant).
Collecting stem cells for a donor (allogeneic) stem cell transplant
You may want to skip this section if you are having a self (autologous) stem cell transplant.
If you are having a donor (allogeneic) stem cell transplant, your transplant coordinator organises a search for a suitable stem cell donor. Anthony Nolan’s video guide shows how a donor is found for donor (allogeneic) stem cell transplants and what happens during the process.
Anthony Nolan video guide to donor stem cell transplants
An allogeneic stem cell transplant is most likely to be successful if your donor’s cells closely match your own. To check this, you have a blood test that looks at proteins called human leukocyte antigens (HLA). Your cells make HLA proteins to help your immune system recognise cells that belong in your body. There are lots of different types of HLA. Your medical team try to find a donor whose HLA types match your own as closely as possible. If possible, they also try to make sure you and your donor have been exposed to the same viruses, although this is less important than HLA-matching.
Brothers or sisters are most likely to have HLA proteins that are similar to yours. Around 1 in 3 people have a brother or sister who is a good match.
If you don’t have any brothers or sisters, or if they are not a good match for you, your medical team search for a volunteer whose HLA type matches yours as closely as possible. Millions of volunteers are registered with national and global stem cell registries. DKMS, a charity that maintains an international stem cell donor registry, has more information about stem cell donation.
A transplant using stem cells from a volunteer is called a ‘matched unrelated donor’ (MUD) transplant. The chance of finding a matched unrelated donor depends on your ethnicity. People of European descent are most likely to find a suitable match. People of black and minority ethnic groups are not well represented in stem cell donor registries and are less likely to find a match. People of rare, mixed ethnicity may find it difficult to find a matched unrelated donor.
If a matched unrelated donor is not found for you, it might be possible to use other sources of stem cells that might not be as close a match. These include:
- A relative (biological parent or sibling), whose HLA type half matches yours: this is known as a ‘haploidentical’ donor. Due to genetics, siblings have a 50% chance of being a half-match to each other.
- Umbilical cord blood from an unrelated donor: Umbilical cord blood does not have to be as closely matched to your HLA type as other sources of stem cells. It is more likely to be used for children than adults because it contains fewer stem cells than other sources. Registers of stored umbilical cord blood are available.
Stem cells are usually collected from the donor’s blood stream (peripheral blood stem cell transplant) or bone marrow (sometimes called a ‘bone marrow transplant’). Donors are given information on what to expect when they donate their stem cells. The NHS website also has helpful information on what is involved in being a donor.
Your transplant team can give you more information about the source of stem cells for your transplant.
High-dose anti-cancer therapy (conditioning)

Conditioning is the high-dose anti-lymphoma treatment you have before your infusion of stem cells. It aims to kill any leftover lymphoma cells in your body and to reduce or destroy the stem cells in your bone marrow. This makes room for the new, healthy stem cells in your bone marrow. If you are having a donor (allogeneic) stem cell transplant, it also helps stop your immune system rejecting the donor cells.
There are different strengths (intensities) of conditioning treatment:
- Full intensity or ‘myeloablative’ treatment involves high-doses of chemotherapy, and possibly radiotherapy, given with the aim of destroying the stem cells in your bone marrow.
- Reduced intensity treatment involves lower doses of chemotherapy, which reduce the stem cells in your bone marrow but do not destroy them completely. You might have reduced intensity treatment if you are not fit enough to have full intensity treatment. It causes less severe side effects than full intensity treatment but it has a higher risk of lymphoma relapsing afterwards.
The conditioning treatment you have depends on:
- your type of lymphoma
- the type of transplant you’re having
- individual factors such as age and any other conditions you have.
Your medical team should explain to you what conditioning treatment they recommend and why, as well as what is involved.
Conditioning usually involves high-dose chemotherapy. How it is given and how long it takes depends on the exact chemotherapy drugs you need. You might also have antibody therapy or targeted drugs. A few people have a form of radiotherapy called total body irradiation (TBI) as part of their conditioning. If you have TBI, it might be given as a single dose or in several doses over a few days.
For lymphomas, the most common conditioning treatment is a chemotherapy regimen called BEAM:
- B – BiCNU® or BCNU or carmustine
- E – etoposide
- A – Ara-C or cytarabine
- M – melphalan.
You have BEAM in hospital over 6 days. The drugs are given through your central line. More information about BEAM and the side effects it can cause is available from Macmillan Cancer Support.
If you are having a donor (allogeneic) stem cell transplant using stem cells from an unrelated or mismatched donor, you may need higher intensity treatment. You might have a different conditioning treatment if you are having an allogeneic transplant using stem cells from umbilical cord blood or from a half-matched relative.
During your conditioning, you also have treatments to help with any side effects you might experience.
Stem cell infusion
You usually have your stem cell transplant (when you are given the healthy stem cells) 1 to 2 days after finishing your conditioning treatment. Your medical team usually call your transplant day ‘day zero’. They measure your recovery time starting from this day.
On the day of your transplant, the stem cells are given to you through your central line, just like a blood transfusion. It is a very straightforward procedure that takes around an hour, depending on the number of bags of stem cells you need to have. You are monitored while the stem cells are given.
Stem cell infusions are generally well tolerated. Occasionally, they can cause side effects such as:
- feeling sick or being sick
- a bad taste or burning feeling in your mouth
- high blood pressure
- allergic reaction
- infection.
Some of these are related to the preservatives used when stem cells are frozen. You are closely monitored for signs of any side effects or reactions and treated for them straightaway. If you have side effects, your infusion might be slowed down.
The day of your infusion can be very emotional. If you find it hard to cope with your emotions, tell your nursing team. They can suggest techniques that might help.
I am still making art about my recovery, and think I always will. It was something that helped to give me a focus out of something so surreal and life-changing.
Waiting for your blood counts to recover (engraftment)
Once the new stem cells are in your bloodstream they make their way to your bone marrow. They then settle into your bone marrow and start dividing to make new blood cells. This process is called ‘engraftment’. Engraftment usually takes 2 to 3 weeks but can sometimes take longer, especially if the new stem cells have come from umbilical cord blood.
While the new stem cells are settling into your bone marrow, your blood counts are likely to be very low, putting you at risk of experiencing serious side effects. Most people stay in hospital so they can be closely monitored until their blood counts have recovered.

Then came the waiting until the donor’s stem cells started to grow within my bone marrow. During this time, I was isolated in my own room and felt a bit like I was just one big lab sample at times! The biggest problem for me was the boredom. I didn’t have the energy or the concentration to read and, although the internet is wonderful, even being online becomes boring after a while. I found the music I have always loved helped enormously. It helped to drown out the bleeping and the air conditioning and it blocked out an empty-feeling echo in the room.
Tell your team if you feel unwell in any way at all.
You are particularly at risk of developing infections due to a very low white blood cell count (neutropenia). Several measures are used to try to prevent this.
If you are staying in hospital while you wait for your blood counts to recover:
- You usually stay in a hospital room on your own. The room is cleaned regularly and sheets and pillowcases are changed every day. You cannot have plants or flowers in the room.
- Hospital staff and visitors must wash their hands before entering your room. They might also need to wear gloves, gowns or aprons, and face masks.
- People shouldn’t visit you if they are unwell. Children might not be allowed to visit at all – although some hospitals allow them to if they are well.
If you are at home while you wait for your blood counts to recover:
- Follow the guidance given to you by your transplant team.
- Take your temperature and check for signs of infection regularly. Contact your medical team immediately if you have a high temperature or any signs of infection.
- Take all the medicines you have been prescribed.
- Look after your central line. Your medical team will show you how to do this.
- Brush your teeth and rinse your mouth regularly with mouth wash.
- Make sure your environment is clean. If you are staying in accommodation arranged by your transplant centre, it should be cleaned and the bedding changed every day.
- Ask friends and family not to visit you if they are at all unwell.
- If you are staying at home and you have any pets, wash your hands after touching them. Don’t let them lick your face and make sure you don’t come into contact with their wee or poo.
If you are staying in hospital or having ambulatory care:
- Wash or shower every day.
- Your medical team monitor you closely for any signs of infection. They take your temperature and pulse, check your oxygen levels, and clean your central line regularly.
- You might be given antibiotics to prevent common infections.
- You might be put on a special diet. This cuts out foods that are likely to contain infection-causing bacteria or fungi. There is limited scientific research supporting neutropenic diets and advice varies between hospitals.
I continued the long recovery from stem cell transplant at home, while getting physiotherapy for my legs and feet and trying to build my body up by eating well and getting more quality sleep.
Infections are very common in the first few weeks after a stem cell transplant, particularly in people who received stem cells from a donor. If you develop an infection, you are treated straightaway.
While you are waiting for your blood counts to improve, you have treatments to support your recovery. You might have:
- Blood transfusions if you have a low red blood cell count (anaemia). Anaemia can make you feel very tired and sometimes short of breath.
- Platelet transfusions if you have low platelet levels (thrombocytopenia). Platelets help with blood clotting. Tell your nurse if you notice any signs of bleeding like blood in your wee or poo, bleeding gums or a nosebleed.
- Treatments for side effects such as a sore mouth, diarrhoea, nausea and vomiting. These side effects are related to your high-dose treatment rather than the stem cell transplant itself.
Some people develop a high temperature, a rash, diarrhoea or fluid retention at around the time of engraftment. This is called ‘engraftment syndrome’. It is more common after a self (autologous) stem cell transplant than a donor (allogeneic) stem cell transplant. It is treated with steroids. However, these symptoms can also be caused by other factors, including chemotherapy.
Once your blood counts have recovered and you are well enough, you can go home. If you’ve had ambulatory care at home, you no longer have to visit the hospital every day for appointments.
After this time, you are followed-up closely by your medical team. You can read more about follow-up and recovery after a stem cell transplant on our pages about self (autologous) stem cell transplants and donor (allogeneic) stem cell transplants.
Watch our 'Recovering from a stem cell transplant' webinar
On 12 July 2023 we held a webinar on recovering from a transplant. Our panel included two nurses who support people through their transplant and two people who have experienced a transplant.
Listen to our podcast where John Murray, Nurse Clinician in Bone Marrow Transplant, and Angie Leather, who is Lead Nurse for Transplant and Haematology CNS, talk about the role of stem cell transplants, when they are used and the important differences between autologous (self) and allogeneic (donor) stem cell transplants. This podcast includes discussions around this often very difficult subject, and contains information on side effects and treatment outcomes that may be potentially distressing.
