Exercise and physical activity
Physical activity (exercise) is important for both physical health and emotional wellbeing. This information is about physical activity before, during and after treatment for lymphoma. It gives tips to help you build physical activity into your day-to-day life in ways that are safe for you.
We have separate information about getting ready for treatment (prehabilitation). We also have resources to help with your physical and mental wellbeing.
On this page
What physical activity should I do?
Frequently asked questions about physical activity and lymphoma
 Benefits of physical activity
Benefits of physical activity
In this video, Lifestyle advisor Jane Mullarkey talks about how to keep active in your day-to-day life.
Physical activity can have lots of benefits. It can help to:
- prepare your body for the most suitable treatment
- reduce side effects of some treatments for lymphoma
- reduce risk of infections while you are on treatment
- reduce the risk of developing blood clots while you are on treatment
- reduce fatigue
- increase muscle strength and improve balance
- control your weight, blood pressure and blood-sugar levels
- reduce the risk of coronary heart disease
- build bone strength to help prevent brittle bones (osteoporosis), which is particularly important for women given treatment that affects their ovaries (such as pelvic radiotherapy). Menopause also increases your risk of osteoporosis.
- improve your general emotional wellbeing, for example by managing stress – some people find it additionally beneficial to be outside and around nature.
Possible benefits of physical activity for people affected by lymphoma
There are lots of benefits to physical activity. For example, the research tells us that it can reduce fatigue and pain. It can also prevent or help with other conditions, as well as helping to prevent the progression of cancer.
Physical activity can have benefits before, during and after treatment for cancer. For example:
- A study looking at people treated with chemotherapy for lymphoma found that doing an exercise or relaxation programme significantly improved quality of life.
- A study looking into the benefits of physical activity in 122 people with Hodgkin and non-Hodgkin lymphoma found that aerobic (cardiovascular or ‘cardio’) activity improved physical abilities and quality of life, including in those people having chemotherapy.
- An analysis of 44 studies (with a total of over 3,000 participants who were living with various types of cancer, including lymphoma) found significantly reduced cancer-related fatigue in people who did moderate physical activity, including some strengthening activity.
- A review of 10 studies of people with blood cancers (including lymphoma) in hospital before having a stem cell transplant found improved heart and lung (cardiorespiratory) functioning in those who took physical activity.
- A review of three studies of people with blood cancers (including lymphoma) found a reduction in fatigue in people who participated in an exercise programme during their hospital stay for a stem cell transplant.
- A review of 100 studies found a lower rate of cancer recurrence (relapse) and fewer side effects of treatment in people who kept up their physical activity compared with those who did very little.
I think exercise always makes you feel better, even if you don't always feel like it. I found a walk to the shops or to the post box was a good way of getting outside and starting to move a bit more without overdoing it.
The NHS website has more information about the health benefits of physical activity.
Your medical team can offer advice about types of physical activity that are safe for you. You might need to avoid certain types for a while or take some precautions when exercising. However, research suggests that taking physical activity before and after treatment for cancer is generally safe and beneficial.
Macmillan Cancer Support publish an evidence-based review about the importance of physical activity for people living with and beyond cancer.
 What physical activity should I do?
What physical activity should I do?
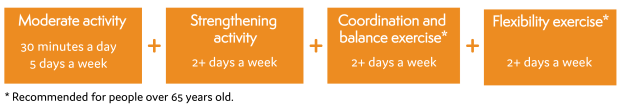
The UK physical activity guidelines are the same for people with cancer who are otherwise well as they are for people who do not have cancer. However, it’s important to be realistic and to do physical activity that is both safe for you, and an appropriate amount – you might need to build up gradually.
For adults, the recommendation is to do 150 minutes (2 and a half hours) of moderate activity in chunks of at least 10 minutes each week. If you prefer, you could instead take 75 minutes (1 and a quarter hours) or brisk (quick and energetic) activity.
The recommendations for children vary according to age and physical ability. Guidelines are available on the UK government website.
As part of your physical activity, a couple of times a week, you should include:
- strengthening activities – examples include reaching up towards the ceiling or sky, and stretching your arms out in straight in front of you
- coordination and balance exercises
- flexibility exercises – particularly for people aged 65 years or over.
You can think of physical activity as ‘working out’ and expending energy through using your muscles. However, it also involves what I call ‘working in’, which focuses on your mind and is just as important. You can get that through things like relaxation, taking some deep breathing, mindfulness and yoga.
Achieving the recommended amount of activity
One way to reach the recommended amount is to do 30 minutes of moderate physical activity 5 days a week. Moderate physical activity makes you breathe more quickly but doesn’t make you feel short of breath.
Some people feel overwhelmed at the thought of taking exercise – I prefer the term ‘physical activity’ as you don’t have to do formal, structured ‘exercise’ to get physical and mental benefits. You can build it into your daily life.
Speak to your medical team about the type and intensity of physical activity that is safe for you. For some people, physical activity is part of their social life. For example, you could play tennis or go for a walk with a friend. For others, physical activity gives an emotional outlet and an opportunity for quiet reflection and mental relaxation.
The main thing is to find a type of exercise you enjoy – that way, you’re more likely to continue doing it over time. After treatment, I thought how important it is to value my time. Eight years on, I continue to do so. My life is much more balanced – I’m careful not to fill every moment with work and to make time for myself and for my family. Once a week, I spend a day with my son and take him swimming. I am more easily able to compartmentalise than I used to be, and not to worry about the things that I can’t change.
Your emotional response to having lymphoma might affect the type of physical activity you choose to do. After a diagnosis of lymphoma, some people feel less confident about their body – for example, in terms of appearance or their physical abilities. Do what feels right for you. This might also mean building up your level of physical activity gradually.
Try to build physical activity into your day-to-day life. For example, take steps instead of a lift or escalator.
For help with adapting exercises (to make them manageable or more challenging), you could ask your GP to refer you to a physiotherapist or cancer exercise specialist.
 Building up gradually
Building up gradually
It’s not necessary or desirable to go straight into doing lots of physical activity if you are not used to it.
Start with small amounts of physical activity and build up slowly. For example:
- You could start with walking 20 minutes, on three days each week.
- After a few weeks, once you feel able to, add another 10 to 15 minutes walk each week.
Thanks to the encouragement of my support group, I started to go circuit training once a week. I was sceptical that I’d be able to do it, but looking back, it was the start of my rehabilitation and physical improvement – there was a time a year earlier that I’d struggled to walk 100 yards. It’s important to be patient with yourself though. Eat well, take rest and build up gradually.
 Types of physical activity
Types of physical activity
Physical activity can be categorised into different groups. In line with the recommendations, you should aim to include moderate activity, strengthening activities and coordination, balance and flexibility activities in your weekly activity.
 Examples of moderate activity include:
Examples of moderate activity include:
- walking
- mowing the lawn
- vacuum cleaning
- gentle cycling
- dancing
- aqua aerobics
- golf.
 Examples of strength activities include:
Examples of strength activities include:
- digging in the garden
- getting in and out of a chair
- squatting
- walking up steps
- carrying shopping bags
- push-ups
- sit-ups
- resistance-band training
- yoga.
 Examples of coordination, balance and flexibility activities include:
Examples of coordination, balance and flexibility activities include:
The NHS website has more examples of different types of physical activities, including suggestions for those you can do at home.
 Safety precautions
Safety precautions
Seek advice about the type and intensity of physical activity that is suitable for you. Your clinical nurse specialist, a physiotherapist or cancer exercise specialist can be good people to ask. They can also advise on any precautions you should take based on your individual circumstances. For example, you might be advised against doing high-impact activity (such as running) if lymphoma affects your bones and you have a higher risk of bone fracture.
During, or soon after your treatment for lymphoma, you might be advised to avoid some activities, particularly if you have certain side effects, including those that lower your blood cell counts.
Low blood counts
Shortage of platelets (thrombocytopenia)
Thrombocytopenia of is a common side effect of chemotherapy and some targeted therapies for lymphoma. Thrombocytopenia can also happen if you have lymphoma that affects your bone marrow.
If you have thrombocytopenia, you are at a greater risk of bruising and bleeding so you should avoid high-impact sports such as football and rugby.
When I was diagnosed, my doctors warned me to be very careful if I was gardening, and to take extra precautions to avoid bruising or injury involving bleeding. This meant that tasks took longer as I was taking time and care to protect myself. I wore thicker gloves, and it was definitely worth the struggle getting my wellingtons on and off!
Shortage of neutrophils (neutropenia)
Neutropenia is a common side effect of chemotherapy. It can also happen if you have lymphoma in the bone marrow. You are also more vulnerable to infection if you have HIV or have had a stem cell transplant (particularly an allogeneic (donor) stem cell transplant) within the last 6 to 12 months.
Be aware of how to limit your risk of infection if you are neutropenic. Check with your medical team for advice. For example, they might recommend that you avoid public swimming pools in certain situations.
Low red blood cells (anaemia)
Anaemia is a side effect of some treatments for lymphoma. It can also happen if you have lymphoma in the bone marrow. Anaemia lowers the amount of oxygen in your blood, making you tired and short of breath. This might affect which types and intensity of physical activity is suitable for you.
Other side effects that can affect which physical activity is suitable for you
Other factors you might need to consider when planning your physical activity include:
- Effects of chemotherapy drugs on your heart or lungs – you might feel short of breath and in discomfort when doing high-intensity exercise. Ask your clinical nurse specialist for advice about what’s safe for you.
- Nerve damage to your peripheral nervous system (peripheral neuropathy) – this can cause symptoms such as muscle weakness, and numbness in your hands or feet. Peripheral neuropathy can affect your grip and balance, so consider the safety of your choice of exercise. For example, instead of cycling outside on a road, you could use a stationary (‘exercise’) bike indoors.
- Diarrhoea or vomiting can happen for lots of reasons, including as a side effect of lymphoma treatments and pain relief medication. It can also be a symptom of heightened stress and anxiety. Diarrhoea and vomiting change the levels of certain minerals (such as sodium and potassium) in your body. This means that you should not exercise while you have diarrhoea or vomiting as this could further affect such levels and make you unwell.
- Bone health – If your bone health is affected by lymphoma or treatment for lymphoma, seek advice from your medical team about the types of exercise that are safe for you.
 FAQs about physical activity and lymphoma
FAQs about physical activity and lymphoma
We offer below some general information about some of the questions people affected by lymphoma often ask about exercise. Speak to your clinical nurse specialist for guidance specific to your situation.
 Is it safe for me to swim in public pools?
Is it safe for me to swim in public pools?
Swimming has many health benefits, including helping to strengthen muscles, increasing your fitness and helping to manage stress. However, there might be times when you should avoid public swimming pools. This includes if you:
- are neutropenic, in order to avoid infection from public pools and changing rooms
- are having radiotherapy, because chlorine could irritate the skin in the area being treated
- have a central line or PICC line (a tube inserted into a vein deep inside you to give treatments and take blood), due to risk of it becoming dislodged or infected.
Should I choose rest over exercise?
Rest is essential in helping you to recover from lymphoma. Even people who haven’t been affected by lymphoma should build rest into their day-to-day life. However, the evidence shows that it is both safe and beneficial to do physical activity during and after treatment for cancer.
Not taking much physical activity can lead to muscle weakness and fatigue. Some people get into a cycle of doing less activity, feeling more tired, so doing less activity and so on. Try to keep up your physical activity levels so that you can continue with your normal activities and to help with your emotional wellbeing.
Tips to help balance physical activity with rest:
- Speak to your medical team for advice about how to get an appropriate balance of physical activity and rest.
- Be kind to yourself – you might not be able to do as much physical activity now compared with before you had lymphoma. For some people, it can take a year or two before feeling fully back to how they were before having lymphoma, so try to show yourself patience.
- Build your level of physical activity up gradually.
- Have regular breaks and give yourself enough time to recuperate afterwards. This should include a ‘rest day’ between any days that you do higher intensity physical activity, when you take more gentle physical activity instead.
You could make a note of the type of exercise you do and how you feel at the time, straight after, and a day or two later. This helps to see how the physical activity sessions affect you – you can then make any changes accordingly.
Can physical activity help to prepare me for treatment?
Physical activity can play an important role in helping to prepare your body for treatment (prehabilitation). This can have lots of benefits, including a shorter stay in hospital and fewer side effects.
Can physical activity help my recovery from treatment?
Physical activity can have a positive impact on recovery from cancer treatment. It might help to:
- shorten recovery time
- prevent physical and mental decline
- lower fatigue and some of the longer-term and late effects linked with some treatments
- improve emotional wellbeing.
Keeping up good fitness levels can have wider-reaching health benefits, including lowering the risk of heart (cardiovascular) disease, brittle bones (osteoporosis) and obesity.
Some people see the end of treatment as a good time to begin a healthier lifestyle. You might be interested in using a gym. If so, some offer programmes specifically for people who are recovering after cancer treatment. There are also trained physiotherapists and exercise specialists who are skilled and knowledgeable in this field. Speak to your clinical nurse specialist for guidance on where to find one.
Can physical activity prevent a relapse (return) of lymphoma?
There is growing support for the potential role of physical activity in lowering the risk of cancer returning (relapsing). Staying active can also increase the likelihood of you being well enough for optimum treatment in the future, should your lymphoma return.
Where can I find out more about physical activity?
Speak to your medical team or GP for advice about the type and intensity of physical activity that is suitable for you.
The British Association of Sport and Exercise Sciences (BASES) also publish a statement on exercise and cancer survivorship.
You might also be interested in our following resources:
- Useful organisations listing, which has a section on physical activity and exercise.
- Live your Life workshops, which is a peer-led self-management course designed for people who have just finished treatment or who are on active monitoring (watch and wait).
- Physical wellbeing resources, which includes videos on exercise and keeping physically active, a tutorial on rejuvenating stretches you can do at home, and a practical toolkit on fatigue and physical exercise.
