Peripheral neuropathy
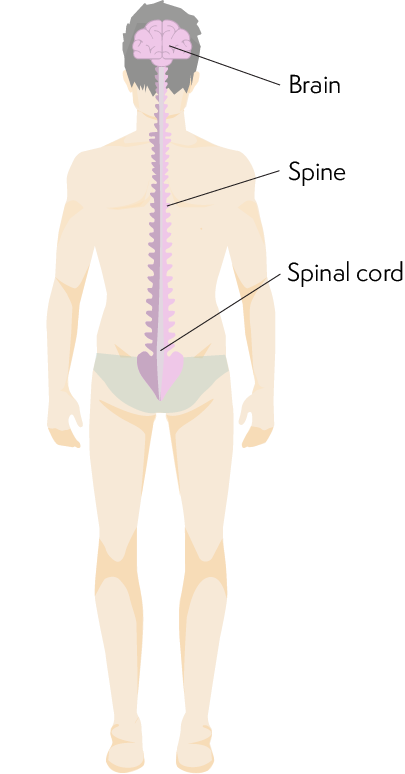
Peripheral neuropathy is damage to the nerves of your peripheral nervous system (network of nerves outside of the brain and spinal cord). It can be a side effect of treatment for lymphoma. Occasionally, it is a symptom of the lymphoma itself. This information gives tips you might like to try to manage any symptoms and prevent further nerve damage.
On this page
What is peripheral neuropathy?
Why do people with lymphoma get peripheral neuropathy?
What is peripheral neuropathy?
Peripheral neuropathy means there is temporary or permanent damage to the nerves of the peripheral nervous system. The nervous system works a bit like a network of electrical wires. Specialised cells (receptors) and nerves within it pick up and carry signals and messages between different parts of your body. However, if you have peripheral neuropathy, this communication is disrupted.
The peripheral nervous system
The peripheral nervous system is made up of the:
- sensory nervous system, which carries information from your skin, muscles and joints, through the spinal cord and to the brain, about the sensations your skin and joints feel (such as heat, pain and touch)
- autonomic nervous system, which carries messages to and from your internal organs (for example controlling blood pressure, heart rate, gut function and bladder function)
- motor nervous system, which carries messages from the brain, down the spinal cord and to the muscles, to tell them to move.
Symptoms of peripheral neuropathy
Symptoms of peripheral neuropathy depend on which nerves are affected: sensory, autonomic or motor. Most commonly, peripheral neuropathy affects the sensory nerves.
If you have symptoms of peripheral neuropathy, tell a member of your medical team. They can take early action to prevent further nerve damage and can offer support with any difficulties you’re experiencing.
Sensory neuropathy
Sensory neuropathy is a type of peripheral neuropathy that affects the sensory nervous system. Common symptoms include:
- pins and needles, numbness or a burning sensation, often in the hands or feet
- pain
- being more or less sensitive to touch
- being more or less sensitive to very hot or very cold temperatures
- unexplained sensations (for example, feeling as though you have something in your shoe when you don’t)
- not being sure where your limbs are without looking at them
- difficulty with tasks that need precise (fine) movements, like doing up buttons, tying shoelaces or opening jars
- ‘restless legs’ (an urge to move your legs).
Symptoms that start in your hands and feet might travel further up into your arms or legs if the neuropathy gets worse.
The chemotherapy I was receiving led to peripheral neuropathy. My treatment needed to be adjusted because the peripheral neuropathy got worse – I could barely feel my hands or feet, and I couldn’t do the things I enjoy, like crosswords or bowling. The peripheral neuropathy lasted for quite a few months, but it gradually improved and I now have very few problems with it; just a coldness in my toes. My hands are fine now and I’m back to bowling and doing the things I love.
Autonomic neuropathy
Autonomic neuropathy is peripheral neuropathy that affects the autonomic nervous system. The most common symptoms of autonomic neuropathy are:
- light-headedness or dizziness when you stand up
- constipation
- tummy (abdominal) bloating
- inability to tell when your bladder is full, which can lead to incontinence
- erectile dysfunction (impotence) in men.
Motor neuropathy
Motor neuropathy is a type of peripheral neuropathy that affects the motor nervous system. Common symptoms of motor neuropathy are:
- muscle twitches, cramps or pains
- muscle weakness, which can make tasks like writing, carrying things and climbing stairs difficult.
Motor neuropathy is not a very common side effect of treatment for lymphoma. However, if you do experience symptoms, you might be referred to a neurologist (doctor specialising in disorders of the nervous system) to check for nerve damage. Your neurologist might do a nerve conduction test and an electromyography (EMG) test. Usually, you have these tests done in one appointment.
Why do people with lymphoma get peripheral neuropathy?
Peripheral neuropathy can be a:
Side effect of lymphoma treatment
The most common cause of peripheral neuropathy in people with lymphoma is when it develops as a side effect of treatment.
Whether you develop peripheral neuropathy depends on which type and dose of drugs you are treated with. If peripheral neuropathy is likely to be a side effect of your treatment, your doctor should discuss this with you before you start treatment.
The drugs most likely to cause peripheral neuropathy are:
- platinum-based chemotherapy drugs, including cisplatin, oxaliplatin and carboplatin
- vinca alkaloids (a group of chemotherapy drugs) including vincristine and vinblastine (included in the ABVD chemotherapy regimen)
- targeted drugs such as bortezomib, thalidomide and brentixumab vedotin.
Chemotherapy-induced peripheral neuropathy (CIPN)
Peripheral neuropathy that is a side effect of chemotherapy is sometimes known as ‘chemotherapy-induced peripheral neuropathy’ (CIPN). CIPN affects the sensory nerves more often than motor or autonomic nerves. It often causes mild symptoms, such as tingling in your hands and feet.
When symptoms start depends on the type of chemotherapy you have; however, symptoms often occur after a few courses (cycles) of chemotherapy. Occasionally, symptoms worsen or start only once your treatment finishes. This is sometimes called ‘coasting’.
I have peripheral neuropathy in my hands and feet, which gives me a sensation like numbness or tingling. It is a really peculiar sensation during the day. At night, it's far worse, but I have a cream containing menthol that I often use, which helps. My medical team tweaked my treatment plan to remove one of the chemotherapy drugs that was causing nerve damage and some other side effects. I was reassured that this would not be disastrous, and that it was important to report side effects. Seven months after finishing chemotherapy the peripheral neuropathy is much improved.
Symptom of lymphoma
Peripheral neuropathy can be a symptom of your lymphoma. This can happen if:
- The chemicals produced by some lymphomas (paraproteins), stick to nerves and damage them. This is quite common, particularly in people with Waldenström's macroglobulinaemia (WM), a rare type of non-Hodgkin lymphoma.
- Lymphoma cells spread into nerves and push up against (compress) them or grow around the tiny blood vessels that supply the nerves. This is rare.
Other conditions or illnesses
Other conditions and illnesses can cause peripheral neuropathy, including diabetes, hepatitis, shingles and low vitamin B12 levels. Drinking a lot of alcohol over a long period of time can also cause nerve damage.
There are also some hereditary conditions that can cause peripheral neuropathy, including Charcot-Marie tooth disease (CMTD) and Hereditary neuropathy with pressure palsies (HNPP).
Having lymphoma and another condition that can cause nerve damage increases your risk of developing peripheral neuropathy. Your medical team consider this when they plan your treatment.
Diagnosis of peripheral neuropathy
Peripheral neuropathy is usually diagnosed through a combination of:
- your answer to questions about your symptoms
- physical examination.
If you drive and you are diagnosed with peripheral neuropathy, you must tell the Driver and Vehicle Licensing Agency (DVLA). You can find information on the UK government’s website about how to do so. There is more information about driving if you have peripheral neuropathy in our frequently asked questions section.
Questions about your symptoms
Your doctor will talk to you about how your symptoms affect your day-to-day life. This might include asking you:
- to describe your symptoms and when you experience them
- how long your symptoms go on for
- whether you experience pain with your symptoms
- whether you feel sick, faint or more tired than usual
- whether you are experiencing any difficulties with bladder control or sexual functioning.
They should also check whether you have any other health conditions and if you are taking any medication for them.
Physical examination
You are likely to have a physical examination as an outpatient. The tests you have might include checking your:
- sense of touch – a reduced or heightened sense could be a sign of damage to your sensory nerves
- balance and coordination, for example, whether you can walk in a straight line – difficulty doing so could be a sign of damage to your motor nerves
- ability to tell where parts of your body are when you have your eyes closed – difficulty could be a sign of damage to a certain type of sensory nerves
- movements (reflexes) in response to being tapped in your ankles, knees and wrists – slow responses could be a sign of damage to your motor nerves
- changes to your blood pressure when you move from lying to standing – a drop could be a sign of damage to your autonomic nerves.
Nerve conduction test (NCT)
In a nerve conduction test, electrodes are put onto your skin. These are small devices that carry tiny electrical shocks (impulses). A specialist doctor (electrophysiologist) checks how quickly and how well your nerves carry the impulses. Very slow or weak signals can be a sign of peripheral neuropathy.
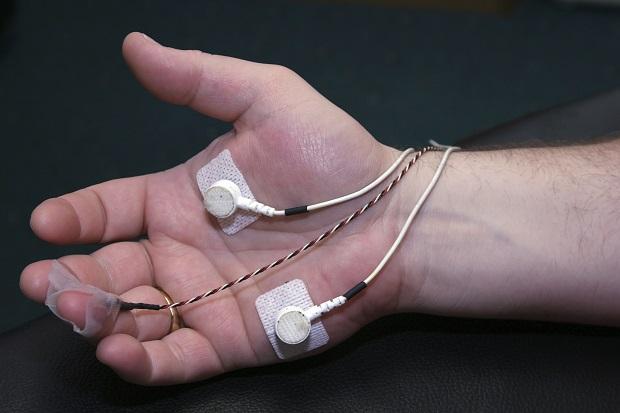
Electromyography (EMG) test
With an EMG test, you have one or more small needles put into a muscle. These send tiny electrical impulses into the muscles. The needle measures how well the muscles respond to the electrical signals. Little or no response could be a sign of peripheral neuropathy.
Treatment for peripheral neuropathy
While there is no way to undo nerve damage, your doctors can help to prevent more damage from happening. Let your medical team know as soon as possible about any symptoms of peripheral neuropathy to give them the best chance of offering effective care.
If your lymphoma treatment causes or worsens peripheral neuropathy, your medical team might reduce the dose or switch you to a different treatment. Further nerve damage can possibly be prevented if you stop or reduce the dose of the drug that is causing it.
If your peripheral neuropathy gets worse very quickly, your doctors might recommend plasmapheresis (plasma exchange). However, this is not used if your peripheral neuropathy is a side effect of chemotherapy. During this process, your blood is filtered to remove some of your plasma (made up of proteins and other substances) with more healthy plasma. Macmillan Cancer Support have more information about plasma exchange.
Treating pain as a symptom of peripheral neuropathy
Some people experience nerve (neuropathic) pain as a symptom of peripheral neuropathy. If pain is a symptom of your peripheral neuropathy, you might be referred to a pain clinic, where a specialist can provide information and might suggest specialist treatments to help manage the situation.
Painkillers such as ibruprofen or paracetamol don’t usually help with pain from peripheral neuropathy. You might be given a medication such as an anti-neuropathic pain drug, which you take by mouth (orally), as tablets. These work in different ways and are often used to treat other conditions.
If your pain is in one or more specific areas of your body, your options might include:
- capsaicin cream (taken from red hot chilli peppers), which you can apply to your skin to help relieve pain in specific areas of your body.
- lidocaine (anaesthetic) plasters, which you stick to your skin on painful areas of your body.
- other topical treatments such as menthol cream and anti-neuropathic treatments.
In some cases, if other approaches are not effective for you, you might be prescribed oral opioid (morphine-like) medication for a short while, in order to control symptoms. However, this is uncommon.
Different approaches work for different people. You might need to try more than one form of pain relief before you find one that works well for you. You might also be interested in trying a complementary therapy, such as acupuncture or mindfulness meditation – these are used as well as any treatments your medical team recommends, not instead of them. If you are interested in trying a complementary therapy, check first with your medical team if it is safe for you, even if it is one you’ve had before.
You might be interested in The British Pain Society’s resources for people living with pain. These include publications that are free to download and patient voices video recordings.
Practical tips for coping with peripheral neuropathy
Below, we offer some tips you might like to try to help you cope with symptoms and to stay safe. We also outline some of the difficulties your medical team can help with.
Coping with symptoms
Speak to your medical team for help to manage any symptoms you experience. Limit your alcohol intake as alcohol can affect nerve functioning. You might also find it helps to wear gloves and thick socks in cold weather, as cold temperatures can worsen symptoms.
I have struggled with peripheral neuropathy (PN) on my hands and feet, which is a particular challenge because I work in a supermarket and sometimes have to handle chilled food. I have found ways to help with this, like using thermal socks and using a heat pack on my hands.
Staying safe
Nerve damage can limit the signals you receive, including sensations of touch, pain and temperature. Without these, you might not realise you’ve hurt yourself. Take steps to avoid such harm, for example:
- Wear gloves to protect your skin from cuts and scratches when gardening and washing-up.
- Protect your feet by wearing shoes that fit well – flat or low-heeled shoes. Seek advice from your pharmacist or GP if you notice redness or rubbing.
- Keep floors and passageways well-lit and free from clutter to avoid tripping over or walking into things.
If peripheral neuropathy affects your sense of temperature:
- Use a thermometer or ask someone else to check the temperature of water in your bath, shower or washing up water.
- Wear gloves in cold weather as you might not realise that your skin is becoming damaged by the cold (frostbite).
Difficulties your medical team can help with
Speak to your medical team about any difficulties you experience so that they can offer support. A good first point of contact is often your clinical nurse specialist.
- If you have pain, muscle weakness or balance problems that make day-to-day tasks difficult, you might be offered a referral to a specialist. For example, a physiotherapist could suggest exercises to help improve your symptoms. They might also organise for you to have equipment, such as a walking stick, to help make life easier. An occupational therapist can make recommendations about adaptations to make around your home and, if appropriate, your place of work.
- If you have constipation that does not ease with diet and lifestyle changes, speak to your GP about the possibility of taking laxatives – do not take these without seeking medical advice first.
- If you experience erectile dysfunction (impotence) as a symptom of peripheral neuropathy, speak to your GP for advice.
The emotional impact of peripheral neuropathy
Whether it’s short-term or long-term, peripheral neuropathy can have a significant effect on your day-to-day life, relationships and emotional wellbeing. You might feel low, anxious, frustrated, experience heightened stress and difficulties sleeping, which can worsen symptoms and make them harder to cope with.
As well as supporting you with practical ways of managing your symptoms, your medical team can also signpost you to sources of emotional support.
You might also want to talk to our information and support team about how your symptoms affect you, physically and emotionally.
Some people find it helps to connect with other people affected by peripheral neuropathy, to share experiences, offer mutual support and suggestions.
- Our helpline team might be able to put you in contact with someone else who has experience of peripheral neuropathy, via our Buddy Service.
- You can read personal stories of others affected by lymphoma and peripheral neuropathy on our website, for example Pam, Pat and Penelope.
Frequently asked questions about peripheral neuropathy and lymphoma
Below are some frequently asked questions about peripheral neuropathy and lymphoma. Speak to your clinical nurse specialist for guidance specific to your situation.
Can I prevent peripheral neuropathy?
Talk to your medical team about lowering your risk of developing peripheral neuropathy. For example:
- If you have experienced peripheral neuropathy in the past, your medical team can take this into consideration when planning any further lymphoma treatment for you. Where possible, they’ll avoid giving you treatments that could cause or worsen peripheral neuropathy.
- If you are lacking certain vitamins from your diet, for example B12, this can increase your risk of developing peripheral neuropathy. Your doctor might make recommendations to increase your intake of B12 or offer dietary supplements.
- If you regularly drink a lot of alcohol, you might be advised to avoid or lower your alcohol intake while you are having treatment for lymphoma. The NHS and the charity Drinkaware both give tips on reducing alcohol intake
- If you have diabetes, it is important to control your blood sugar levels, in order to reduce your risk of developing peripheral neuropathy.
Will my peripheral neuropathy go away?
For most people, symptoms of peripheral neuropathy improve over time, although they can go on for months or even years. For some people, symptoms continue permanently. There is a higher likelihood of symptoms going on for a long time with more severe symptoms of peripheral neuropathy.
With Waldenström's macrogolublinaemia, neuropathy often starts to improve once you begin treatment for the lymphoma.
My peripheral neuropathy seems to be worsening. Does this mean my lymphoma is coming back or getting worse?
Some people in remission wonder if a worsening of symptoms of peripheral neuropathy are a sign that their lymphoma is coming back (relapsing). This is very unlikely to be the case. If you are worried, speak to your clinical nurse specialist so that they can offer reassurance and, if appropriate, arrange for you to have any tests or scans.
Why should I tell the DVLA if I’m diagnosed with peripheral neuropathy?
If you drive and you are diagnosed with peripheral neuropathy, you must tell the Driver and Vehicle Licensing Agency (DVLA). This is so that they can consider whether they believe it is safe for you to continue to drive while you are experiencing peripheral neuropathy.
You can find information on the UK government’s website about how to tell the DVLA, what happens after you tell them, and about possible outcomes, for example, if you need to have your car or vehicle adapted, or if you need to stop driving for a while.
