Lymphoma treatment for people with other health conditions
The treatment you have for lymphoma depends on your individual circumstances. Treatment might be adapted for people who have other long-term health conditions or who are not able to have the standard treatment options.
We have separate information on lymphoma and HIV, lymphoma in people who have had an organ transplant (post-transplant lymphoproliferative disorder) and lymphoma during pregnancy.
On this page
Lymphoma and long-term health conditions
Lymphoma treatment and other health conditions
Lymphoma and long-term health conditions
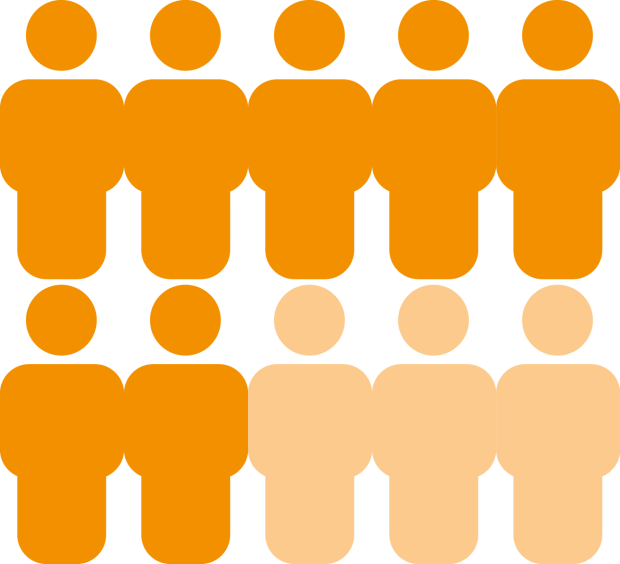
Long-term health conditions can affect people of any age, but they become more common as you get older. Older people are also more likely than younger people to develop cancer, including many types of lymphoma. This means it is common for people to have another health condition as well as lymphoma.
Some of the common long-term conditions you might have as well as lymphoma include:
- high blood pressure
- diabetes
- heart disease
- respiratory disease
- kidney problems
- arthritis
- HIV
- dementia
- mental health problems
- another type of cancer.
You might have another condition that is not on the list.
It is important for your medical team to know about any other conditions as some lymphoma treatments can put extra strain on your organs.
Lymphoma treatment and other health conditions
Having another medical condition might affect your treatment for lymphoma. For example:
- Some illnesses can affect how well organs such as your heart and lungs work. These illnesses might increase your risk of developing side effects from some lymphoma treatments. If your organ function is reduced, you might need to have the doses of treatment you receive adjusted.
- Problems with your kidneys or liver could affect how your body deals with some of the medicines used to treat lymphoma. This might mean you need different treatment options or lower doses of your treatment.
- Medicines you take for other conditions might react with certain lymphoma treatments. This might mean you need a different treatment, or a lower dose of treatment.
- Some conditions might make it difficult for you to take some types of medicines. For example, you might not be able to swallow tablets or open medicine bottles without assistance.
- Other conditions might affect how well you are able to follow your treatment plan (for example, if you have problems with your concentration or memory).
Your medical team consider all these factors when they recommend the most appropriate treatment for your lymphoma. They aim to offer you treatment that has the best chance of successfully treating your lymphoma with the fewest possible side effects or long-term effects on your health.
Before deciding on the best approach for you, your medical team might recommend that you have extra tests to find out if you are fit enough to receive certain treatments. For example, you might have tests to find out how well your heart or kidneys are working.
Looking after other health conditions when you have lymphoma
It is important to look after your other health conditions and make sure you are as fit as possible before you start lymphoma treatment. Tell your medical team about any conditions you have and all the medications you are taking, including those you take without a prescription such as vitamins and supplements.
Some medications can cause problems if they are given together. If you are on any medicines that might interfere with your lymphoma treatment, your medical team might:
- suggest changing the medicines you usually take
- adjust the dose of your medicines
- monitor you carefully for any signs that your lymphoma treatment and your other medicines might be affecting each other.
If you are under the care of another specialist, they will work with your lymphoma team to make sure you get the most appropriate treatment for your lymphoma and any other condition you have.
While undergoing treatment my type 2 diabetes was controlled with insulin, but I was able to return to an alternative medication afterwards.
Some treatments for lymphoma might also make a difference to your other health conditions.
After six cycles of chemotherapy, I was pronounced in remission. Not only that, but my rheumatoid arthritis (RA) was now amazingly well controlled and I discovered that a faulty protein on the B-cells in my immune system had been responsible for both my RA and lymphoma. I was therefore offered rituximab, which had been part of my chemo, to control my RA. It is delivered twice a year by infusion. Other than a tiny dose of an oral steroid this is all I need to be much more mobile at 76 than I was at 40!
Lymphoma treatment and age
As you get older, your organs might not work as well as they used to even if you don’t have any other health conditions. For example, your liver, kidneys, immune system, bone marrow and heart might not work as well as they did when you were younger. This makes you more likely than a younger person to experience side effects of treatment.
However, this varies a lot from person-to-person. Age on its own is not a good indication of how well your organs work. This means your choice of treatment is not based just on your age. Your medical team consider your overall health, including how active you are and how well your organs are working, and will organise investigations to assess this.
If you are fit enough, they are likely to recommend the same treatment options they would for a younger person. If they have concerns about your fitness or the health of your organs, they might run extra tests. They will adapt your treatment to suit your individual needs based on your test results which assess how well your organs are working.
Older people are also more likely to have practical issues, such as difficulty getting to and from the hospital. You might need someone around to care for you and help you with day-to-day living. This can be difficult if you live alone. Tell your medical team about your circumstances so they can help you find the support you might need whilst undergoing treatment, and once you have finished your treatment.
Adapting treatment to your needs
Lymphoma treatment might be adapted for people who have other conditions or who are not fit enough to have standard treatment. Our information on different types of lymphoma has more detail on the different treatment options for each type of lymphoma.
Goal of treatment
The goal of lymphoma treatment depends on the type of lymphoma you have. It also depends on factors that affect how well treatment works or your risk of experiencing side effects. For example, being older or having another long-term condition could have an impact on how effective some treatments are. It could also increase your risk of experiencing side effects. This might change the overall goal of treatment for you.
Depending on the type of lymphoma you have, the treatments you are able to tolerate and your personal feelings, the goal of treatment might be to:
- Send the lymphoma into remission: This typically requires intensive treatments that might not be suitable for everybody.
- Keep the lymphoma under control for as long as possible: This might be possible with gentler treatments.
- Give you a good quality of life: In this case, treatments with a lower risk of side effects might be more appropriate.
- Relieve and control your symptoms: This is known as palliative care.
Your medical team will talk you through all your options. They will discuss how effective the treatment is likely to be, the side effects you might experience, and what you hope to get from the treatment. This should help you decide on the most suitable treatment plan for you.
How might treatment be adapted?
When your medical team recommend a treatment plan for you, they always consider:
- the benefits of the treatment (how well it is likely to work)
- the risks of the treatment (the side effects it might have and the impact of these on your quality of life).
Having another health condition or being less fit could change the balance of risks and benefits. For example, the risk of side effects might outweigh the benefits of a particular treatment. If this is the case, your medical team consider how they might change or adjust your treatment plan to reduce the risks. There are different approaches they might consider.
- Lower doses: If you can’t have the standard dose of treatment, you might be able to have the same drugs at a lower dose. For example, CHOP (a combination of chemotherapy drugs often used to treat lymphoma) can be given in lower doses if necessary. This is sometimes called ‘mini-CHOP’.
- Fewer or different drugs: You might not be able to have certain drugs if you have heart or lung problems. If this is the case, some drugs might be swapped for different options, or left out of your treatment altogether. For example, bleomycin is often left out of ABVD chemotherapy for people with lung conditions.
- Fewer cycles of treatment: If you are not able to tolerate the standard course of treatment, your medical team might suggest that you have a treatment that requires fewer cycles. This might be followed by radiotherapy instead of the extra cycles of chemotherapy. Some people might have a longer interval between treatment cycles to give their body longer to recover.
- Gentler treatment options: There are lots of different chemotherapy options, and your doctor might suggest a less intensive option if you have other health conditions.
- Different way of having treatment: Treatment with chemotherapy tablets you take at home might be an option for some people.
- Monotherapy: Your medical team might recommend treatment with just one drug instead of a combination of several. This is called monotherapy. It could be a chemotherapy drug that can be given on its own, or an antibody therapy such as rituximab.
- Targeted drugs: For some types of lymphoma, targeted drugs are available that might be suitable for people who are older or who are unable to receive the usual chemotherapy treatments. Targeted drugs generally have fewer side effects than chemotherapy.
- Radiotherapy: Some people might have a course of radiotherapy to control their symptoms instead of more intensive treatment to get rid of the lymphoma.
Saving treatment until you need it
People whose lymphoma is not causing problems do not always need treatment straightaway. Many people with slow-growing (low-grade) lymphomas that are not interfering with their day-to-day life have periods where they can be monitored without treatment. This is known as ‘active monitoring’ or ‘watch and wait’.
Active monitoring saves you from side effects or late effects of treatment for as long as possible. Many slow-growing lymphomas are kept under control for many years with active monitoring, only needing treatment from time-to-time.
Other considerations
Some people are able to have the usual treatment for their type of lymphoma, but might need to make other adjustments. For example:
- medications you are on for your other health conditions might be changed or temporarily stopped
- you might need additional treatments to support your body through your lymphoma treatment, such as blood transfusions or growth factors to keep your blood counts healthy
- you might need to be admitted to hospital for your treatment, or be monitored more regularly than usual.
Additional support
Some people do not need changes to their treatment, but might require other types of support. For example:
- You might have an illness that makes it hard to understand what is happening. We have EasyRead books that use simpler words and pictures to explain about lymphoma. Or you could talk to a friend or family member about what is going on.
- If you have a condition that affects your mobility, you might need help with everyday things such as transport to appointments, shopping or childcare. Ask your medical team what support is available to help you manage.
- You might have a condition that makes it difficult to open medicine bottles or to remember to take your tablets at the right time. If so, you could ask a friend or family member to put your medication into a tablet organiser (or other box with sections). Some pharmacies also offer this service.
- Occasionally, your lymphoma team might refer you to other specialist teams to assess your organ function and optimise any other medical conditions before you start treatment.
- If you have a carer, they might find our information on caring for someone who has lymphoma helpful. Carers UK and Carers Trust also offer information and support. Macmillan Cancer Support have information about caring for people who have dementia and cancer.
Understanding your treatment options
It is important that you are comfortable with the treatment plan your medical team makes with you. Remember that they need to understand your personal circumstances and your thoughts on treatment. Tell them about the medicines you are taking, any health problems you have, any support you might need and what is important to you.
Ask all the questions you need to make sure you understand the risks and benefits of your treatment. You could take a list of questions with you to your appointment so you don’t forget to ask anything. If you are concerned that the treatment might not be effective or you are worried about possible side effects, tell your medical team.
There can be a lot to take in. You might find it helpful to take someone to your appointments with you to talk through it all afterwards. You could take notes or ask the doctor or nurse to write things down to help you remember. You might want to ask them if you can record what they say so you can listen back later.
