Mark
I'm not seeking 'recovery', as I don't expect to go back to where I started. I view my experience of CAR T-cell therapy as a form of restoration and 'renaissance'.

My lymphoma story began in 2018, I was 62. I am married to Diane with three grown-up children; one moved back to live with us during this time. I was working as a specialist endodontist in dental practice and teaching the subject (root filling teeth) to postgraduate students at Manchester University Dental Hospital, working full weeks and finding life both busy and rewarding in so many ways. At the time I can remember thinking that everything was ‘coming together’ - professionally and in life as a ‘whole’.
We are a close-knit family and are happy to share our life-experiences. Di and I feel very blessed to have such a close relationship with our children. They have been a great support during the last 19 months.

I had taken up running five or six years previously and found it a good stress reliever and great fun. Di and I are keen to remain fit and over previous holidays we had walked up the highest peaks in Wales and Scotland, Snowdon and Ben Nevis. To celebrate Diane ceasing to work on Mondays (she is a hygiene therapist working in Practice and teaching too) we decided to climb the highest mountain in England this time, Scafell in the Lake District. We did so! However this success was followed later that day with an unscheduled, unprotected night out on this mountain due to a navigational mishap! It was a most painful experience and one we look back upon as a reference point in our lives. There is a saying ‘what doesn’t kill you makes you stronger’! This experience has been a ‘benchmark’ for comparison, particularly recently in relation to the ‘journey’ having medical treatment, chemotherapy and in particular to CAR T-cell therapy.
Our experience on Scafell peak was a most painful experience. It has been a 'benchmark' for comparison, particularly recently in relation to having medical treatment, chemotherapy and in particular to CAR T-cell therapy.
I had not visited a doctor since I was a teenager, but was struggling with abdominal pain, of which I had become aware in Autumn 2018. I noticed around this time and particularly after the Manchester half marathon in October, at training sessions at the running club, it was harder and harder to maintain previous form. Eventually in December Di suggested we attend our local medical practice for help. She knew instinctively something was wrong and over ruled my tendency to allow ‘things to find their own place’. With hindsight, a less than clever attitude, ignoring warning signs! I didn’t mention a small swelling I had noticed above my left clavicle, it seemed insignificant at the time and totally unconnected with my ‘gut’ pain, which was coming intermittently, but at times quite uncomfortably.
In early December, my GP arranged for some blood tests as an initial approach to help determine the cause of the symptoms. Having had a number of blood tests during the weeks leading up to Christmas, the results were delivered on New Years Eve which indicated I was suffering from chronic kidney disease!
You could have knocked me down with a feather! An abdominal ultra sound scan was arranged. In the meantime a ‘chance’ conversation with a Consultant friend resulted in him arranging a visit to a Kidney specialist at the same hospital. My friend felt I was too fit to have kidney disease, and ‘something didn't add up’!
His colleague having done further blood tests and a thorough examination, including an ultrasound scan expressed concern that my kidneys were causing a problem, though they were not the prime cause of my developing illness, which included some altered sensation in my right leg. The kidney problem was part of a ‘bigger picture’.
Friday, 11th January 2019 was a life-changing ‘watershed’; it was the last day I worked as I was admitted to hospital as an urgent case for investigation. My usual busy routine was about to cease and I was to have to ‘let go’ and allow events to unfold. The kidney specialist said ’it would be a ‘bumpy ride’, but I would be in good hands as an in patient’, and help could be sought more urgently as an in-patient. He spoke with reassuring tones, however it was ‘a look in his eye’ that expressed a concern that told me I needed immediate help for something that he couldn’t fully explain.
The next two weeks were a venture into the unknown. I had a series of further daily blood tests (often at 6 am each morning!), a lumber puncture, bilateral nephrostomies (drains inserted into each kidney to enable more efficient function) a full body CT scan, an MRI scan, ECG and heart ultrasound scan and a biopsy taken from an enlarged lymph node just above my left clavicle. A preliminary diagnosis of non-Hodgkin B cell lymphoma was made. Subsequently I was placed on a high dose of oral steroids to start a breakdown of the tumours.
The world ‘out there’ doesn’t stop despite one’s personal circumstances changing! Di made a visit each and every day despite being busy at work, and our children visited most days, often with ’goodies’ for the staff as well as ourselves. Despite the shock of the event, we were going to make the best of this situation as a family. Another highlight during this two-week period was to accompany our practice, our ‘extended family’ to a ‘musical’ as part of our Christmas celebrations. It was a colourful musical interlude for a few hours from the hospital routine.
The diagnosis was refined as a diffuse large B-cell non-Hodgkin lymphoma with underlying follicular lymphoma (which I could have had for years!)
The diagnosis was refined as a diffuse large B-cell non–Hodgkin lymphoma (DLBCL) with underlying follicular lymphoma (which I could have had for years!). I was reassured that treatment for DLBCL was given with a ‘curative intent’, and that it would start straight away with R-CHOP chemotherapy. Initially this was delivered via an intravenous catheter, however, a PICC line (peripherally inserted central catheter) was placed (painlessly and without event by a talented nurse practitioner) beneath my left upper forearm, to enable easier intravenous drug delivery. When asked by my Consultant if I wanted to know the prognosis for my condition, I responded, reminding her of our earlier conversation when she made it clear that treatment is given with ‘curative’ intent. That was all I needed to know. I just had to ‘will’ this to be the case!
From the outset I determined a number of principles; I was not going to ‘feel sorry for my self’, self-pity is a negative state of mind and a damaging emotion. Knowing instinctively that we can ‘project our future’, a positive approach to life is more likely to give a desired outcome. You can’t deny that there is an element of fear in the ‘unknown’, however my approach is to acknowledge it and then move-on with a more positive frame of reference. Another important fact is to avoid ‘labels’, such as the term ‘cancer’ with its many negative connotations, so I have used the term illness or disease, or just the term ‘lymphoma’, and have allowed the listener to ‘fill in’. At no time have I wanted to be a ‘victim’ of the problem, I suppose what I am saying is I wanted to take ‘ownership’ and ‘responsibility’ for the state I found myself in. Finally, and very importantly I have avoided the use of the term ‘recovery’ – this implies returning to a previous ‘status-quo’, and that certainly would not be possible, or even wise! Hence the term ‘restoration’ or even ‘renaissance’ – ‘rebirth’!
The first course of chemotherapy is usually administered as an in-patient to ensure a safe tolerance of the drug regime. In addition it ensured my kidney function was improving. This had been the principle-presenting symptom due to an abdominal obstruction caused by the lymphoma, restricting urine flow to my bladder. The drains inserted into each kidney enabled more normal function. The only down side to this was to have to wear two leg bags to collect the urine, and over the next few months I suffered a number of urinary tract infections. A small price to pay for a ‘ticket to live’!
We make small positive steps amidst the fear and unknown as we get to grips with an illness, but each positive step is a milestone towards restoration. We depend utterly upon the wisdom and expertise of the doctors and nurses who attend us. Once we establish trust and knowledge with them of the ‘journey to health’, we are going a long way to helping ourselves to get better! Significant in this journey has been the love and support of Diane and my children. They have been a source of inspiration and great comfort. One realises where life’s priorities really lie.
We depend utterly upon the wisdom and expertise of the doctors and nurses who attend us.
After two weeks, I was allowed home. Hooray! This was a relief to myself and my family, no more daily hospital visits, a good 20 mile round trip. However, within 72 hours I developed a high temperature and was re-admitted, and given a course of IV antibiotics and more daily early morning blood tests! 5 days later I was relieved to be back at home.
In the early days in hospital amidst many of the unknowns, life does go on, strangely almost, a reassuring ‘imposter to the party’. I had been President-elect to the British Endodontic Society and was due to take up ‘office’ at a national meeting in London in March 2019. I had previously arranged speakers for this meeting; however, I still had much to do to secure the speakers for the Regional Meeting in Manchester in November 2019. Prednisolone is a wonderful drug! However, it stops you sleeping when given as an immediate high dose, as I was experiencing. So, highly energised as I was, I spent a number of ‘charged late nights’ emailing friends and contacts to arrange speakers for the November conference. I was grateful for the opportunity that the Prednisolone offered in giving me the energy to get on with this. The result was a line up of 5 international guest speakers and 4 ‘home-grown’ from the UK. This was a very positive distraction from the ‘hospital-oriented life’ I was living with, and to some extent kept me in contact with ‘the world outside’ and my previous reality.
The five remaining scheduled sessions of R-CHOP chemotherapy were given subsequently as an ‘out-patient’ at three weekly intervals and ended in mid-May 2019. There was always the most positive ‘banter’ with the nursing staff and fellow patients in these sessions, very much part of the ‘therapy’! A PET scan (positron emission scan – radioactive glucose is picked up by actively dividing cells and show as a ‘hot-spot’) showed an ‘equivocal’ response. A further PET scan three weeks later demonstrated some resolution, however, active disease was still present. During this time it was possible to remove the left nephrostomy, however there was still some restriction to the flow from the right kidney, so this drain was replaced. Hard to believe, but the whole procedure was carried out without any form of analgesia, and to my delight and astonishment, without pain, an amazing experience!! The next day, I peaked a temperature of 38.50C, was experiencing a bacteraemia, so an emergency visit to the casualty department resulted in a two day admission and the need for intravenous antibiotics.
At the end of June 2019, my Consultant explained that they were going to change my chemotherapy regime to R-ICE, suitably named ‘salvage therapy’! If anything is going to help you feel as though you are on the ‘scrap-heap’ of life, this was it! I insisted that it be called by another name! This was to involve a further three cycles, this time as an inpatient Monday to Friday at the start of each cycle (again 3 weekly intervals), after which I would have an autologous (my own cells) stem cell transplant. A few days prior to the first cycle of this new therapy, a PICC line (peripherally inserted central line) was placed skilfully and painlessly under local anaesthetic to the inner aspect of my left upper arm to deliver the chemotherapeutic agents more centrally.
Between these two courses of treatment, I remember going for a run for the first time for 6 months. I ran on a path between two fields of wheat lined by the most beautiful wild flowers. The sight of this, associated with the freedom to run was a truly moving moment, a moment of ‘real life appreciation’.
After the second R-ICE cycle, I had a further PET scan in early September. Again, the conclusion was of an ‘equivocal' response and it was determined that further R-ICE and stem cell transplant would not be therapeutic. Another form of therapy was to be sought.
My Consultant spoke to me about the option of CAR-T cell therapy. I wouldn’t be able to have this new treatment at my usual hospital, but would need to be transferred to a larger centre where this could be given. She explained that because I came to treatment as a fit individual, I would be a likely candidate for this therapy, however, I would need to be assessed and ‘put forward’ for consideration. CAR T-cell therapy is not an automatic ‘right of passage’.
I recalled at the time how I had recently seen national news coverage on the television of the first lymphoma patient to have had successful CAR T-cell therapy on the NHS. I hadn’t realised at the time that this might be an option for myself. Currently in the UK, if two previous courses of chemo-therapy have not resulted in remission, then CAR T-cell therapy is an option, providing the individual is of a certain level of fitness and any other co-morbidities can be managed.
A consultation was arranged to discuss the possibility of CAR T-cell therapy based at one of the largest single-site oncology centres in Europe. We are very lucky to live so close to this centre of contemporary excellence. This certainly was a momentus meeting, and one that would have great significance to my health outlook. I was accompanied again by my wife Diane, as I have been to all my appointments. She is a wonderfully supportive soulmate; we have been married for 35 years!
Those to whom we are closest have to bear an equally uncomfortable journey of unknowns when we are ill. In fact, I wonder whether their journey is even more difficult than ours as a patient?
Those to whom we are closest have to bear an equally uncomfortable journey of unknowns when we are ill. In fact, I wonder whether their journey is even more difficult than ours as a patient? Theirs is full of the uncertainties we are experiencing, attending, living alongside, wanting to help, but not being able to do more than watch, support and be a ‘shoulder to cry on’ if necessary. We, the patients just have to go with the flow and accept our treatment, as if in the centre of the wheel of activity. I recognise that the support I have had, both from Diane, and from my three grown up children, and indeed a large and concerned ‘greater family’ of friends has been instrumental upon my maintaining a positive and optimistic outlook thorough out this ‘journey’. Those of us who are ill and have such support are more than well blessed!
So, I felt it was with great privilege that I was to be considered for this new contemporary treatment, CAR T-cell therapy. What enormous advances have been made in science; we really are standing on the shoulders of giants, aren’t we? There are 7 centres in the UK for adult treatment of DLBCL and I was the ninth patient to have had this treatment at the centre that I attended. Privileged indeed!
So, I felt it was with great privilege that I was to be considered for CAR T-cell therapy. What enormous advances have been made in science; we really are standing on the shoulders of giants, aren't we?
Early in all this treatment a good and learned friend, a Professor, who knows me well suggested that I avoid consulting the Internet regarding matters medical. He reckoned I would only scare myself! Rather, his advice was to go with the flow and trust the wisdom of those looking after me. Wise and sound in the circumstances, so despite my relative medical knowledge, I determined to allow events to unfold in their own time. I didn’t search the Internet about CAR T-cell therapy until it was offered, and even then it was to gain the bare facts.
We had a break from treatment for about two months after the second R-ICE from the end of August until October. During this time my PICC line was removed. A further appointment to the radiology department confirmed patency of my right ureter, so the remaining right nephrostomy was removed too, this time under AB cover to prevent a risk of systemic infection. I believe ensuring normal kidney function without the inherent risk of intervening bladder and UTI infections due to the nephrostomies was necessary before CAR T-cell therapy could be entertained. It felt like we were on ‘hold’ during this time. It was lovely to be ‘tube-free’! Additionally I had a further biopsy of a swelling that had appeared just in front of my right ear to assist and confirm the diagnosis, plus a further heart scan to ensure there was a ‘baseline’ of cardiac function before treatment.
My T cells were harvested towards the end of October 2019. One is well prepared for this event by the wonderful team who specialise in this care within what is called the Apheresis unit within the haematological department. Despite having been warned that I might require a femoral vein catheter, come the day, the nurses attempted ‘normal’ canulation in a vein in my arm. I found it interesting to observe that larger bore needles give no more discomfort than smaller ones, and minor at that. The secret is not to anticipate or to expect pain. One is rarely disappointed if this is the case!! Allow whoever to do what they have to do, and when they are about to insert the needle, breathe in! Magic! You experience little discomfort!
Unfortunately my veins were ‘not playing’ and only allowed an insufficient rate of blood flow to keep the aphoresis machine ‘happy’. I was given a femoral vein catheter, again a procedure like many others under skilfully given local anaesthetic. Painless and dare I say it another interesting procedure to add to the list! This enabled a sufficient rate of blood flow, which over the next 4 -5 hours allowed my total blood volume to be filtered two and a half times! The machine estimated a 5 litre body volume, so once it had filtered 12.5 litres, the 148mls of harvested white cells was deemed sufficient!
I understand the cells are suitably stored and protected and whisked off by courier. I was told they travel to the USA via Amsterdam where they arrive within a couple of hours. They are forwarded onto the USA within 24 hours where the magic of CAR T-cell transformation begins. Pending the T-cell return, I was given a further course of chemo-therapy to maintain the status quo, this time orally. We went away for the weekend in our caravan, knowing it might be a while before we would get the opportunity to go away again. This was the 9th course of chemo.
They (my cells) are forwarded onto the USA within 24 hours where the magic of CAR T-cell transformation begins.
In March, 2019 I was able to give a presidential address to the British Endodontic Society in London, just between Big Ben and Buckingham Palace. The grand building belonging to the Institute of Civil Engineers sits on the route of the last half mile of the London Marathon! Having done this race a couple of times, the parallel of ‘pacing’ and ‘running the course’ is not lost upon my reflections of coping with this illness and the associated treatment!! The date for the meeting fell well within the treatment sessions between the second and third cycle of R-CHOP treatment. I was without hair, but I ‘fed’ off the atmosphere and the ‘energy’ of the day and felt well! Similarly, the November meeting in Manchester was to have occurred two days before my T cells were to be returned. By some curious ‘bend of time’, without moving the dates, the return was deferred by a week! This meant I was fully able to host the Regional event with an attendance of over two hundred dentists. Such activities are a real therapy in themselves!
The week before the T cell return (which is usually after 4 weeks) it is necessary to reduce the body’s natural defensive response so a further course of chemo is given. In order to deliver this and subsequent intravenous medication and to assist with blood tests a central or Hickman line is required. This was skilfully placed by another nurse practitioner, who having done this many times before was able to successfully carry this out without pain, fuss or any form of trauma whatsoever. She even allowed Di to watch who said it was interesting seeing my neck being cut!!!! Three days of intravenous chemo as an outpatient were interrupted by a weekend ‘off’ followed by admission to the bespoke isolation ward at the hospital on December 9th 2019.
Later that day the CAR T-cells were delivered back to me after five weeks, having been genetically modified on the other side of the Atlantic! There were four nurses involved in the procedure and correct and rigorous checks were made to ensure the right cells were being redelivered. It was dramatic! They are brought in in what looks like a milk churn! They are stored at -70oC in a polystyrene container within liquid nitrogen. Thick insulating protective gloves are necessary when withdrawing the frame containing the bag of cells, around 160mls of milky looking fluid, life promoting ‘self’ returning to ‘self’.
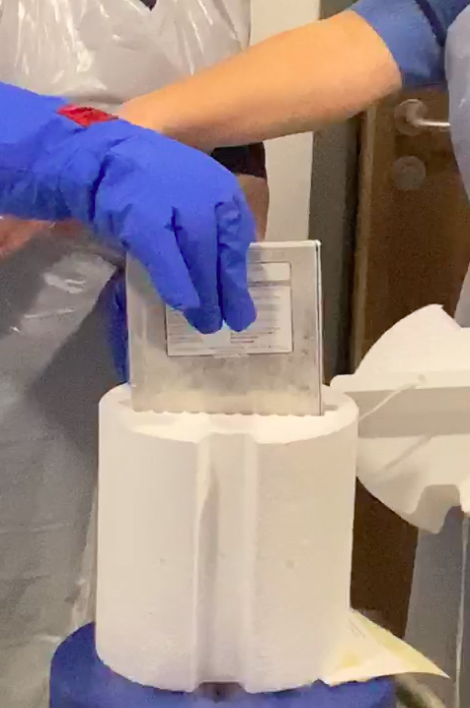
The cells are stored in an agent that prevents cell damage at low temperature. Normally freezing tissues and cells causes cell rupture and death, however, the agent used, DMSO (dimethyl sulfoxide) prevents this. The bag of cells is placed in a water bath at body temperature. Once at this temperature they are delivered via the central line and a drip. The whole procedure took around 8 minutes from thawing to completion of delivery. What was curious was I was immediately aware of a slightly ‘rotting vegetable’ taste. Others in the room could smell ‘sweet corn’ over the next few minutes as the infusion took place. I was ‘breathing off’ the DMSO preservative. Diane said she was aware of this smell for about 24 hours! The procedure was very dramatic and swift, with a ‘degree of high drama’ and then there was a sense of anti-climax once it was over!
For the next six days I acclimatised to isolation in a bespoke and very well equipped room with a lovely view of trees and a sky that spoke of the current weather and at a time of year where the days are shorter and the hours of darkness greater. The ‘rules’ of the ward stipulated no more than two visitors at a time under very strict cross infection rules. Often however, there would be more folk in the room at times, such was the kindness and the flexibility of the staff on this ward. It was a joy to have Diane and all three of our grown up children there with me as a family when possible!
These first six days left me thinking I was experiencing a placebo effect! I felt no different. Daily questions are asked as a routine post CAR T therapy to check for neurological complications, such as where one is, what day of the week it is, being asked to point to various things in the room, counting backwards from a 100 in tens, even in sevens, plus writing a short sentence to check one’s neurological responses. At this time it seemed unnecessary. However, around the sixth day I developed a high temperature, I felt unwell and slowly my energies seemed to drain away day-by-day. The tests are designed to check for neurological changes in co-ordination and cognition. My hand tended to shake as days went by, I noticed how my fine motor control had diminished. Interestingly, as well at this time, a previous small swelling on my right cheek increased in size over a few days. It signalled a need for further scans and tests which were carried out with due haste. With hindsight it seemed like a ‘lymphoma swansong’. The swelling disappeared as quickly as it, had appeared, but more completely. The CAR T cells were evidently at work! Christmas was approaching, celebration and holiday time, I just wasn’t interested. It was a tough time for Diane, who was making efforts to work and visit every day. What a testing time for her this was, however she always appeared with a reassuring smile!!
Around the sixth day I developed a high temperature, I felt unwell and slowly my energies seemed to drain away day-by-day.
This response is expected and is ascribed to an effect called cytokine release syndrome (CRS), where the CAR T-cell treatment causes an immune reaction in the body, a graft versus host type of response. It can be very severe necessitating admission to the intensive care unit. Fortunately I avoided this! However I did feel unwell, at times, very unwell. Just to go to the loo required much effort of will to get out of bed, sometimes taking 20 minutes. It was also assumed the high temperature could relate to infection, so massive doses of IV antibiotics were given which in turn lead to a disturbance of my gut flora, hence ‘the runs’ and the odd accident along the way!! Every few days additional blood was being taken to culture to check for infection too. There were times when I felt as though my ‘life force’ was so diminished; perhaps this is what it feels like when you are dying?
Thankfully this was not the case!! The staff continued to look after me professionally and kindly. I made an effort most days to chat to all who entered my room, whether they were there to clean the room, as they did twice a day, or to change my bedding, or to deliver food and meals. My interest in food was no reflection upon the good fare they offered, I just didn’t have an appetite.
I had a number of profound and wonderful encounters with members of the pastoral team at the hospital. It added to the affirmation that is endemic within the organisation and workforce within the establishment. In addition I enjoyed a number of foot massages, offered as complimentary therapy within the department. It is more than evident that health care is not just about looking after our bodies, but also our minds as well, as exemplified here. The ward even had a visit from a couple of football players from the local Premiership team!
I was in hospital from 9 December 2019 until 3 January 2020, a year on from the original diagnosis. I have, and continue to have routine checks at weekly or bi-weekly intervals. The last two PET scans have shown that all aberrant lymphoma tissue has been eradicated. At present my white blood cell and neutrophil counts remain low. A bone marrow biopsy (another interesting and virtually painless experience, once again performed by another talented nurse practitioner) showed an absence of further disease. It is expected that this will resolve naturally in the next six months.

During this period of regular visits for blood tests and awaiting results, we would leave the hospital for a short walk to our local ‘Maggie’s Centre’. There are 27 such centres in the UK, and three internationally. Maggie’s is a charity providing free cancer support and information in centres across the UK and online. It was a short five-minute walk (ten minute stroll!). Such centres host Support Specialists, Psychologists and Benefits Advisors for patients, their families and friends. It allows time and space for all involved with cancer to share experiences with others in a similar situation around a kitchen table in a centre, or in an online community. There is a peace and serenity here, which is difficult to describe, but very real and very life-supporting. I would recommend anyone going through treatment to visit such a centre given the opportunity.
I have been home for six months now and the COVID virus, which was just peeking over the horizon when I first went in, is firmly part of our lives now. Self-isolation is a necessary way of life having a less than fully functional immune system. I know I will never be the same person after this experience; I don’t use the term ‘recover’ as I mentioned before, but wish to grow and move on, I now want to embrace the new life I have. I look forward to a return to work once this is possible, though perhaps at a less strenuous level. In the meantime we have time to tend to our bees along with many other projects and hobbies!

My family have been wonderful throughout this experience, and are enormously protective of me. They won’t even allow me to answer the front door for fear of infection. I do have to go into hospital for regular blood tests and some treatment, currently on a weekly basis. I also currently take anti-viral, anti-fungal and antibiotic medicines to help give additional protection while my bone marrow and body is returning to normal, but I have found all these things very do-able.
I can't express enough the gratitude I have for everyone involved in my care. My wife and three adult children have been fantastic and the care I have received from the healthcare teams within the NHS has been outstanding.
I can’t express enough the gratitude I have for everyone involved in my care. My wife and three adult children have been fantastic – they have suffered because they have felt so helpless at times. And the care I have received from the healthcare teams within the NHS at both hospitals in which I’ve been treated has been outstanding; I am enormously grateful to them all. This included an 8 week course on meditation whilst waiting for CAR T-cell therapy. I can recommend this whole heartedly!
Exercise has been a big part of my return to health and I am back to running on a daily basis, which is bringing so many benefits both physically and emotionally. I have a deferred ‘good for age’ place in the London Marathon rescheduled for 4th October 2020, C-19 permitting. It is my intention to complete the course, the time is not important, however, the fund raising is! I wish to pay back in a small but significant way for all the love and care that has allowed me to have a second chance.
Would I swap places with anyone? No, not at all, despite the many hospital visits, stays and procedures necessary to encourage my health, it has been a valuable insight into the deeper aspects of life, which dare I admit; we take for granted much of the time. Is the journey to, and through CAR T-cell therapy as scary and as painful as an unscheduled night out on a snow-covered mountain like Scafell? No, not even close! What CAR-T has given is hope, opportunity and life, and it will be a continuing ‘journey’. We stand ultimately upon the shoulders of giants who have focussed wisdom and knowledge and extended the boundaries of our understanding of immunology in order that we may continue life’s potential and to live it more fully.
Thank you to these pioneers and to all who have made this possible, and finally my love and admiration go to Di who has walked every step of this ‘journey’ by my side!
